Contents
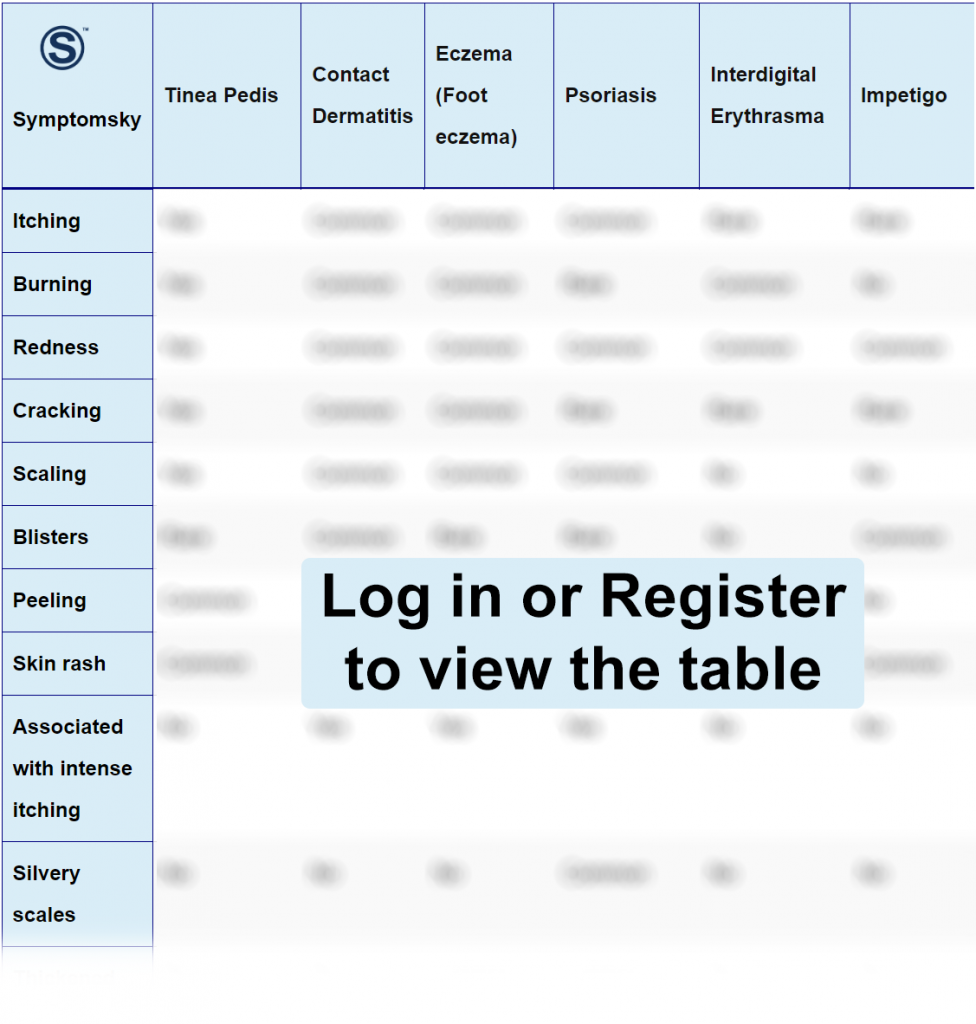
- 1 Tinea Pedis Differential Diagnosis Table:
- 2 How To Distinguish Tinea Pedis From Other Diseases
- 2.1 Distinguish Contact Dermatitis from Tinea Pedis – Diagnosis
- 2.2 Distinguish Foot Eczema from Tinea Pedis – Diagnosis
- 2.3 Distinguish Psoriasis from Tinea Pedis – Diagnosis
- 2.4 Distinguish Interdigital Erythrasma from Tinea Pedis – Diagnosis
- 2.5 Distinguish Impetigo from Tinea Pedis – Diagnosis
- 2.6 Distinguish Cellulitis from Tinea Pedis – Diagnosis
- 2.7 Distinguish Plantar Keratoderma from Tinea Pedis – Diagnosis
- 2.8 Distinguish Planta Pustulosis from Tinea Pedis – Diagnosis
- 3 Important Red Flags With Tina Pedis
Tinea Pedis Differential Diagnosis Table:
Tinea pedis, also known as athlete’s foot, has afflicted humanity for centuries. The first report was by Whitfield in 1908. It is a dermatophyte (fungi) infection of the soles of the feet and interdigital spaces. It is most commonly caused by Trichophyton Rubrum, a dermatophyte initially endemic only to a small region of Southeast Asia, parts of Africa, and Australia.
Tinea Pedis is common in people whose feet have become very sweaty while confined within tight-fitting shoes, and it is contagious. Commonly, Tinea Pedis patients describe pruritic, scaly soles and often painful fissures between the toes. Less often, patients describe vesicular or ulcerative lesions. Some Tinea Pedis patients, especially elderly persons, may simply attribute these scalings to dry skin.
During an examination of the foot, the signs noted depend on the type of Tinea Pedis the patient has, and this could either be Interdigital type Tinea Pedis, characterized by erythema, maceration, fissuring, and scaling, most often seen between the fourth and fifth toes; there is usually pruritus. Chronic Hyperkeratotic Tinea Pedis presents with chronic plantar erythema with slight scaling to diffuse hyperkeratosis. There could be pruritus or not.
Inflammatory/Versicolor Tinea Pedis is characterized by painful, pruritic vesicles or pustules or bullae, most often on the instep or anterior plantar surface; the lesion may rupture.
Ulcerative Tinea Pedis is characterized by rapidly spreading vesiculopustular lesions, ulcers, and erosions typically in the toe spaces.
How To Distinguish Tinea Pedis From Other Diseases
Distinguish Contact Dermatitis from Tinea Pedis – Diagnosis
Contact dermatitis is an allergic skin reaction caused by exposure of the skin to irritants (allergens), which could be cosmetics, fragrances, jewelry, or plants. The rash often shows up within days after exposure and is characterized as pruritic papules/vesicles on an erythematous base. Lichenified pruritic plaques may indicate chronic forms of the condition.
- In contrast with Tinea Pedis, the successful treatment would depend largely on the identification of the substance causing the reaction, and it clears off within 2-4 weeks after elimination of the allergen.
Distinguish Foot Eczema from Tinea Pedis – Diagnosis
Foot eczema refers to a group of skin conditions that cause itchiness and inflammation on the feet. It can also present with blistering or rough/cracked skin.
- Foot eczema could either be: Contact irritant dermatitis/Status disease usually on the dorsal surface of the feet,
- Dyshidrotic/pompholyx: usually on the plantar surface of the feet and between toes.
- Stasis Dermatitis occurs on the legs but also on the dorsum of the feet.
- Unlike Tinea Pedis, foot eczema is an allergic reaction, and treatment will depend largely on eradication of allergen and use of topical steroids.
Distinguish Psoriasis from Tinea Pedis – Diagnosis
Psoriasis is an autoimmune condition that causes inflammation of the skin. It could affect varied areas of the body and is named as such. It could be plaque, inverse, guttate, pustular, erythrodermic psoriasis, sebopsoriasis, or nail psoriasis. The symptoms include patches of thick red, itchy, and scaly skin patches.
- The scaling in psoriasis is much more severe than that of Tinea Pedis, and it can affect many more body areas, including the feet, contrasting with Tinea Pedis, which is confined to the feet.
Distinguish Interdigital Erythrasma from Tinea Pedis – Diagnosis
This is a skin lesion that presents as well-defined pink or brown patches with fine scaling and superficial fissures between the 3rd, 4th, and 5th toe web spaces. Mild itching may also be present.
- It could easily be confused for Tinea Pedis by the characteristic affection of the 3rd, 4th, and 5th toes web spaces, as Tinea pedis commonly affects the 4th and 5th toe web spaces, sparing the 3rd most of the time.
Distinguish Impetigo from Tinea Pedis – Diagnosis
Impetigo, also called school sores, is an acute highly contagious skin infection caused by gram-positive organisms, especially Staphylococcus aureus and Streptococcus pyogenes, affecting the superficial layers of the epidermis.
- The clinical features include red sores on the face and extremities, predominantly affecting infants and children.
- This disease is mainly a secondary infection of a prior skin lesion such as abrasion from trauma, rash from insect bites, scabies, herpes simplex, chickenpox, or eczema, unlike Tinea pedis that is De Novo caused by a fungal infection.
Distinguish Cellulitis from Tinea Pedis – Diagnosis
This is a common, potentially fatal bacterial skin infection. It usually affects the lower legs but can also occur on the face, arms, and other parts of the body.
- The body parts affected usually appear as swollen, painful, red, and warm, and the patient may have fever and chills.
- Unlike Tinea pedis, there’s no scaling.
Distinguish Plantar Keratoderma from Tinea Pedis – Diagnosis
This condition is also known as Keratosis plantaris, and it presents as marked thickening of the soles of the feet. It could be an inherited or acquired condition.
- In contrast to Tinea pedis, it affects more of the sole of the feet and can also affect the palms (in this case called Keratosis palmaris).
Distinguish Planta Pustulosis from Tinea Pedis – Diagnosis
This is a common skin disorder, characterized by recurrent eruptions of fluid-filled pustules or blisters on the feet.
- The lesions appear first as tiny blisters with yellow pus; they eventually turn brown and scaly and cause painful cracks on the skin, making walking uncomfortable.
- It can also affect the hands, unlike Tinea Pedis.
Important Red Flags With Tina Pedis
Tinea Pedis is a fungal infection that has varied clinical presentation depending on the type peculiar to a patient. Its symptoms may mimic another disease process. For example, the interdigital type tinea pedis presents with symptoms closely resembling interdigital erythrasma, etc. As such, it is possible for an inexperienced health care provider or medical officer to miss the exact diagnosis of Tinea pedis.
This makes it necessary for patients presenting to the health care facility, particularly for the first time, to be attended to preferably by a specialist/dermatologist or a medical professional with sufficient knowledge to make the correct diagnosis. So as to proffer timely and appropriate treatment to the patient as well as save cost and reduce hospital stay/time. And this will be achieved by a detailed history, thorough physical examination using bright light (preferably daylight), carrying out investigations such as skin scraping, etc., and prescription of appropriate drugs.
