Contents
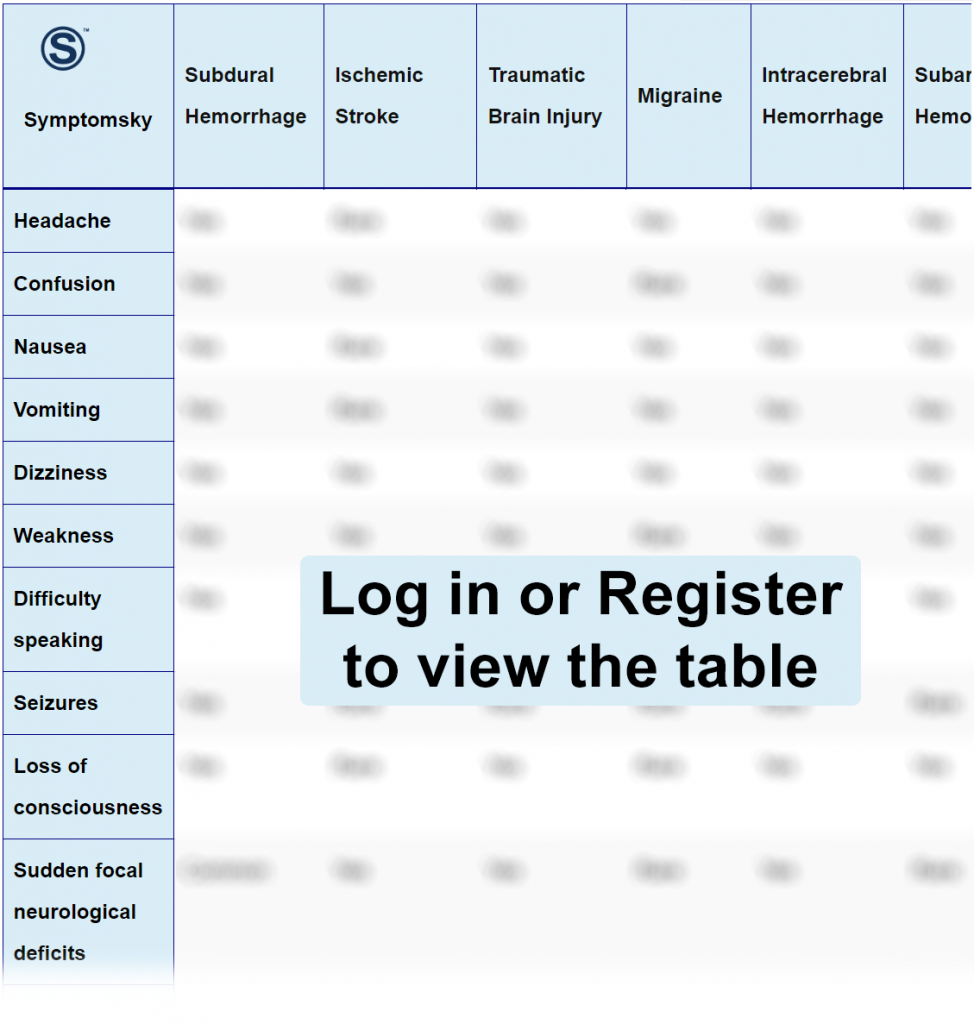
- 1 Subdural Hemorrhage Differential Diagnosis Table:
- 2 How to Distinguish Subdural Hemorrhage from Other Diseases
- 2.1 Distinguish Ischemic Stroke from Subdural Hemorrhage – Diagnosis
- 2.2 Distinguish Traumatic Brain Injury from Subdural Hemorrhage – Diagnosis
- 2.3 Distinguish Migraine from Subdural Hemorrhage – Diagnosis
- 2.4 Distinguish Intracerebral Hemorrhage from Subdural Hemorrhage – Diagnosis
- 2.5 Distinguish Subarachnoid Hemorrhage from Subdural Hemorrhage – Diagnosis
- 2.6 Distinguish Epidural Hematoma from Subdural Hemorrhage – Diagnosis
- 2.7 Distinguish Encephalitis from Subdural Hemorrhage – Diagnosis
- 2.8 Distinguish Brain Tumor from Subdural Hemorrhage – Diagnosis
- 3 Common Red Flags with Subdural Hemorrhage
Subdural Hemorrhage Differential Diagnosis Table:
The brain mass is located inside the skull. Inside the skull and on the brain, there are three layers called meninges whose function is covering and protecting the brain. The outermost layer is inside the skull, it’s a fibrous hard layer called dura mater, inside the dura mater there is a layer called arachnoid, and the innermost layer of the brain is called pia mater. Inside the meninges, there is cerebrospinal fluid which acts as a buffer.
The subdural hemorrhage is an accumulation of blood that occurs between one of the envelopes of the brain that is called dura mater and the brain itself. When there is a subdural hemorrhage, the blood is filtered between the dura mater and arachnoid layers. This blood accumulates inside the outer rigid lining of the brain. The bleeding comes from a blood vessel that breaks within the space that surrounds the brain. This usually happens due to a head injury which can be mild but the blood can cause pressure on the brain, damage the tissues, and produce symptoms.
The most common cause of a subdural hemorrhage is a head injury either due to an accident, a fall, or an attack. It can also happen in aging patients due to cerebral atrophy, patients taking anticoagulants, or due to the loss of cerebrospinal fluid. There are different types of subdural hemorrhage that will be classified according to the time of onset of the symptoms, the amount of bleeding, and brain damage.
They are classified as acute, subacute, and chronic. This means that a subdural hemorrhage may occur within the first 24 hours after an injury or it can even last up to days to weeks for the symptoms to appear.
It is important to emphasize that the symptoms can occur immediately or develop later. Among the symptoms that may occur in a subdural hemorrhage are: Imbalance, confusion, dizziness, headache, nausea, vomiting, fainting, seizures, aphasia, weakness, or numbness.
How to Distinguish Subdural Hemorrhage from Other Diseases
Distinguish Ischemic Stroke from Subdural Hemorrhage – Diagnosis
Ischemic Stroke occurs when there is an interruption in the blood supply that goes to the brain causing the death of cell tissue in the area where it occurs.
- Ischemic Stroke is due to the obstruction of an artery while Subdural Hemorrhage is due to a fracture that affects a vein in the brain.
- Subdural Hemorrhage symptoms can occur even days after the event while Ischemic Stroke manifests itself suddenly.
- Ischemic Stroke symptoms are: weakness or paralysis of one hemibody, loss of sensitivity of one hemibody, facial paralysis of the affected side, asthenia, while Subdural Hemorrhage symptoms are confusion, dizziness, headache, nausea, vomiting, fainting, seizures, aphasia, weakness or numbness.
- Ischemic Stroke surgical treatment, unlike Subdural Hemorrhage, consists of angioplasty to permeate the blocked arteries.
Distinguish Traumatic Brain Injury from Subdural Hemorrhage – Diagnosis
A Traumatic Brain Injury occurs after a shaken impact on the head which causes the brain to hit inside the skull, it stretches and damages some brain cells.
- Traumatic Brain Injury, although it may be due to a stabbing object, most cases are due to an impact that causes the brain to shake, unlike Subdural in which there is a fracture that breaks a vein causing a hemorrhage.
- Traumatic Brain Injury symptoms will depend on the severity and brain damage, the symptoms that go from milder to severe are: headaches, buzzing in the ears, problems with memory and concentration, brief consciousness, severe headache that does not go away, loss of coordination, dragging talk while Subdural Hemorrhage symptoms are confusion, dizziness, headache, nausea, vomiting, fainting, seizures, aphasia, weakness or numbness.
- Unlike Subdural Hemorrhage, most cases of Traumatic Brain Injury are due to the movement of the brain inside the skull, most do not require surgery, relaxants, antidepressants, stimulants, and anxiolytics are given, as well as rehabilitation therapies.
Distinguish Migraine from Subdural Hemorrhage – Diagnosis
Migraine is a chronic disease of the central nervous system with episodic manifestations.
- Migraine is characterized by recurrent episodes of unilateral incapacitating headache that are accompanied by nausea or phonophobia and photophobia while Subdural Hemorrhage headache is insidious and generally accompanied by other symptoms such as vomiting, fainting, seizures, aphasia, weakness, or numbness.
- Migraine has a predominance of the female sex unlike Subdural Hemorrhage that has a predominance of male sex.
- The etiology of Migraine is made up of many theories, most point out that it is related to life habits such as diet, quality of sleep, and exercise, unlike Subdural Hemorrhage that the most common cause is after a traumatic event in which a fracture breaks a vein and triggers the condition.
- The diagnosis of Migraine, unlike Subdural Hemorrhage, is merely clinical.
Distinguish Intracerebral Hemorrhage from Subdural Hemorrhage – Diagnosis
Intracerebral Hemorrhage is the accumulation of blood inside the brain.
- In Intracerebral Hemorrhage, the blood can accumulate anywhere in the brain while in Subdural Hemorrhage, it accumulates under the dura mater.
- The most common cause of Intracerebral Hemorrhage is untreated chronic arterial hypertension while the most common of Subdural Hemorrhage is due to car accidents or falls (aging patients).
Distinguish Subarachnoid Hemorrhage from Subdural Hemorrhage – Diagnosis
Subarachnoid Hemorrhage is the accumulation of blood between the arachnoid and dura mater.
- In Subarachnoid Hemorrhage, the blood is of arterial origin while in Subdural Hemorrhage, it is of venous origin.
- Subarachnoid Hemorrhage is due to causes which are the rupture of an aneurysm or vascular malformations unlike Subdural Hemorrhage which the most common cause is due to car accidents or falls (aging patients).
- Subarachnoid Hemorrhage is more frequent among people between 40 and 60 years old, unlike Subdural Hemorrhage, which is more common in people over 60 years of age.
- Subarachnoid Hemorrhage, unlike Subdural Hemorrhage, has a sudden clinic of very intense headache and vomiting, photophobia, and stiffness of the neck.
Distinguish Epidural Hematoma from Subdural Hemorrhage – Diagnosis
Epidural Hematoma is the accumulation of blood between the skull and the dura mater.
- In Epidural Hematoma, the blood is of arterial origin while in Subdural Hemorrhage, it is of venous origin.
- Epidural Hematoma, unlike Subdural Hemorrhage, does not present changes in behavior, personality, or difficulty walking and maintaining balance.
Distinguish Encephalitis from Subdural Hemorrhage – Diagnosis
Encephalitis is the inflammation of the brain.
- Encephalitis, unlike Subdural Hemorrhage, is caused by viruses.
- Encephalitis, unlike Subdural Hemorrhage, affects young adults and children under the age of one.
Distinguish Brain Tumor from Subdural Hemorrhage – Diagnosis
Brain tumor is a mass located in the brain.
- Brain tumor squeezes a part of the brain causing symptoms while in Subdural Hemorrhage, there is a difference in pressure due to the presence of fluid (blood) that should not be there.
- Brain tumor, unlike Subdural Hemorrhage, depending on their location, will cause focal neurological signs.
Common Red Flags with Subdural Hemorrhage
The people who have a higher risk of having a Subdural Hemorrhage are people who practice high-impact sports, elderly patients, patients with previous brain injuries or brain tumors, patients under anticoagulants treatment. In pediatric patients, they may occur in those who suffer violence or in the shaken baby syndrome.
The diagnosis of Subdural Hemorrhage is based on clinical examination and the findings of a CT, which is the presence of a half-moon-shaped isodense or hypodense image in the cerebral parenchyma.
For Subdural Hemorrhage, the indicated treatment is surgical treatment. It can be done through two surgical procedures, which are: Surgical drainage: enter through a hole in the skull to cerebral parenchyma where the hemorrhage is aspirated. Craniotomy: is made by removing a part of the skull to access the hemorrhage, which is more invasive.
The prognosis will depend on the size of the hemorrhage, location, the speed of the symptoms, and how fast medical assistance was provided. If the patient undergoes surgery in the presence of early symptoms, the rate of recovery without neurological sequelae is very high.
Since most of the Subdural Hemorrhages occur due to brain trauma, the best way to prevent these is to avoid blows in contact sports such as boxing. Also, take good care when having an aging relative doing things such as bathing in order to prevent a fall. It’s important to take preventive measures when driving a two-wheeled vehicle such as a bicycle or motorcycle wearing a protective helmet as well as when doing work with a high risk of head injuries, use safety equipment. Talk to your family doctor if you use anticoagulants and have any of the symptoms of subdural hemorrhage.
