Contents
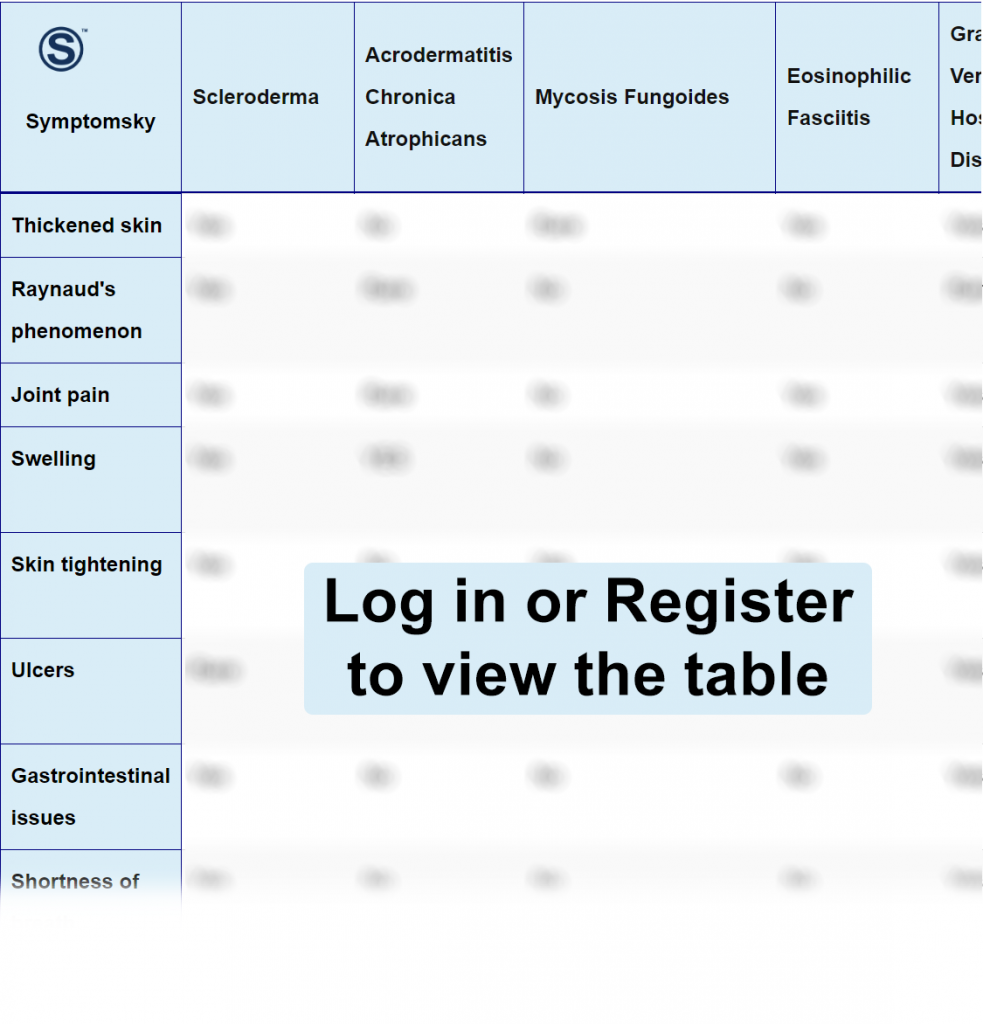
- 1 Scleroderma Differential Diagnosis Table:
- 2 How To Distinguish Scleroderma from Other Diseases
- 2.1 Distinguish Acrodermatitis Chronica Atrophicans from Scleroderma – Diagnosis
- 2.2 Distinguish Mycosis Fungoides from Scleroderma – Diagnosis
- 2.3 Distinguish Eosinophilic Fasciitis from Scleroderma – Diagnosis
- 2.4 Distinguish Graft-Versus-Host Disease from Scleroderma – Diagnosis
- 2.5 Distinguish Complex Regional Pain Syndrome from Scleroderma – Diagnosis
- 2.6 Distinguish Nephrogenic Systemic Fibrosis from Scleroderma – Diagnosis
- 2.7 Distinguish Primary Biliary Cholangitis from Scleroderma – Diagnosis
- 2.8 Distinguish Primary Pulmonary Hypertension (IPAH) from Scleroderma – Diagnosis
- 2.9 Distinguish Eosinophilia-Myalgia Syndrome (EMS) from Scleroderma – Diagnosis
- 3 Important Red Flags in Scleroderma
Scleroderma Differential Diagnosis Table:
Scleroderma is an autoimmune disorder that causes the skin to thicken and become hard. Cells inside the body called fibroblasts live longer and produce much more collagen and protein, which builds up, causing these symptoms in the skin.
Scleroderma is classified into local scleroderma, which involves mainly the skin and the tissue underlying it only, and systemic scleroderma, which involves the skin and internal organs too. The latter can be further classified into limited and diffuse scleroderma according to the degree of involvement of the skin.
Scleroderma is a chronic disease with no cure till now; treatment can only ease up and manage symptoms and the progression of the disease.
How To Distinguish Scleroderma from Other Diseases
Distinguish Acrodermatitis Chronica Atrophicans from Scleroderma – Diagnosis
Acrodermatitis Chronica Atrophicans (ACA) is a late stage of Lyme disease that is manifested by skin rash that can progress very rapidly and chronically to skin atrophy and neurological symptoms.
- Serology using ELISA or western blot shows positive IgG of Borrelia is the gold standard test for diagnosis.
- A positive PCR for Borrelia is also diagnostic for ACA.
- Skin biopsy is rarely needed.
Distinguish Mycosis Fungoides from Scleroderma – Diagnosis
Mycosis fungoides is the most common type of cutaneous T-cell blood lymphoma, where T cells inside your body become cancerous although the skin lesion that appears is not cancerous. The first sign that appears is usually skin rash.
Mycosis fungoides can be easily mistaken for other skin conditions like psoriasis.
- The most diagnostic test for mycosis fungoides is skin and tissue biopsy; several biopsies may be required.
- Dermoscopy can help in differentiating mycosis fungoides from other inflammatory skin conditions.
- T-cell receptor gene rearrangement is often used to detect changes in the gene responsible for T-cells.
Distinguish Eosinophilic Fasciitis from Scleroderma – Diagnosis
Eosinophilic fasciitis is a rare autoimmune condition that affects the connective tissue in which the skin becomes swollen and inflamed and eventually becomes thickened and hard. This usually happens because of the accumulation of white cells; eosinophils.
- A biopsy of the whole affected skin, including deep connective tissue, is the main diagnostic test.
- Sometimes MRI may be used, but it’s not preferred as the biopsy.
- Some blood tests like eosinophilic blood count and erythrocyte sedimentation rate can be done.
“Eosinophilic fasciitis looks like scleroderma, and differentiating between them is often hard, but a very unique difference is the involvement of fingers and Raynaud’s symptoms in scleroderma and their absence in eosinophilic fasciitis; another thing is that eosinophilic fasciitis often responds well to treatment like corticosteroids unlike scleroderma.”
Distinguish Graft-Versus-Host Disease from Scleroderma – Diagnosis
Graft versus host disease is a bad response from your body to stem cell transplantation, often the body recognizes the new stem cells as foreign bodies and starts attacking them, leading to a severe inflammatory response in the body. The symptoms include severe skin rash and some systemic symptoms in GIT, especially causing nausea, vomiting, and diarrhea.
- Diagnosis of graft versus host disease is typically by the clinical presentation of the symptoms that appear a few days after hematopoietic stem cell transplantation.
- Several biopsies of different organs may be needed to confirm and monitor the prognosis of the disease since different organs can be affected.
- Blood tests may be needed since most people develop low blood count with GVHD.
Distinguish Complex Regional Pain Syndrome from Scleroderma – Diagnosis
Complex regional pain syndrome (CRPS) is severe pain that usually affects an arm or a leg after physical trauma. CRPS usually happens when the pain lasts more than the usual recovery time. It’s classified into two types: either type 1 or type 2, both are the same except in type 2, it’s accompanied by nerve damage.
- Budapest Criteria, which were developed to help in the diagnosis of CRPS, showed high specificity for the disease.
- MRI and X-ray can be used to rule out any other muscle problems.
“Diagnosis of CRPS mainly depends on excluding any other causing factors when the time of pain exceeds expected recovery time.”
Distinguish Nephrogenic Systemic Fibrosis from Scleroderma – Diagnosis
Nephrogenic systemic fibrosis (NSF) is a rare condition that affects people with renal problems when they are exposed to a contrast dye containing gadolinium, resulting in fibrosis and thickening of the skin. Internal organs can also be affected, such as the lungs and heart. NSF can look very much like scleroderma.
- A skin biopsy is the main diagnostic test for nephrogenic systemic fibrosis.
- A history of MRI with contrast and advanced kidney disease.
Distinguish Primary Biliary Cholangitis from Scleroderma – Diagnosis
Primary biliary cholangitis is a liver disease in which the common bile duct becomes inflamed and gradually destroys it, leading to a buildup of bile in the liver, which eventually leads to liver cirrhosis and failure.
- Antimitochondrial antibodies are the serological marker in primary biliary cholangitis, which is present in around 95% of patients.
- Elevated liver enzymes and alkaline phosphatase can help in diagnosis.
- In most cases, a liver biopsy may be needed to evaluate the stage of liver failure.
- Ultrasound of the abdomen and, in some rare cases, MRI may be required.
“Primary biliary cholangitis and Primary sclerosing cholangitis are very similar with one major difference: in scleroderma, that disease involves extrahepatic ducts, while in primary biliary cholangitis, it involves only intrahepatic.”
Distinguish Primary Pulmonary Hypertension (IPAH) from Scleroderma – Diagnosis
Primary pulmonary hypertension is an idiopathic disease that causes narrowing in arteries in the lung, leading to increasing blood pressure. IPAH is a chronic disease with no cure till now. The disease usually develops very slowly, and most people don’t experience any symptoms for years, making IPAH very hard to diagnose early. Progression of IPAH can lead to many problems, including heart failure.
- Right heart catheterization involves doctors inserting a small tube with a balloon to directly measure pressure inside the lung.
- Echo or ECG are used to determine any abnormalities in the heart or any changes that may have occurred as a complication of the disease.
- Perfusion lung scan is a radiological test that can help see the changes that have happened in the arteries of the lung and whether a clot may have formed, causing the disease.
“Other diagnostic imaging tests like X-ray or MRI may be performed to detect any abnormalities that may have caused the disease. Scleroderma can also cause pulmonary hypertension in about 40% of patients, but differentiating between the two diseases commonly happens by the appearance and confirmation of other symptoms in scleroderma, like skin thickening that doesn’t occur in IPAH.”
Distinguish Eosinophilia-Myalgia Syndrome (EMS) from Scleroderma – Diagnosis
Eosinophilia myalgia syndrome (EMS) is a rare condition that is caused by the digestion of a high amount of L-tryptophan, causing the body to produce more eosinophils that build up in the body, causing several symptoms affecting many organs. The most common symptoms are muscle pain, shortness of breath, and skin rash.
- A history of the digestion of large amounts of L-tryptophan, together with a blood test that shows a high level of eosinophils plus muscle pain, is usually a major indication of the disease.
- A high level of CK can help in diagnosis since it indicates damage to muscles.
“In some cases, Scleroderma may also present with eosinophilia, which happens in a small percentage of people, but differentiation between the two diseases is simple by measuring the blood level of L-tryptophan.”
Important Red Flags in Scleroderma
Scleroderma is a very hard condition to live with, especially with no cure present. A lot of therapies are available to help control symptoms and increase the quality of life. Some people may need stem cell transplantation or surgery when the disease progresses very badly to ease their symptoms. There are a lot of patient education programs and group therapies for scleroderma patients that may help.
