Contents
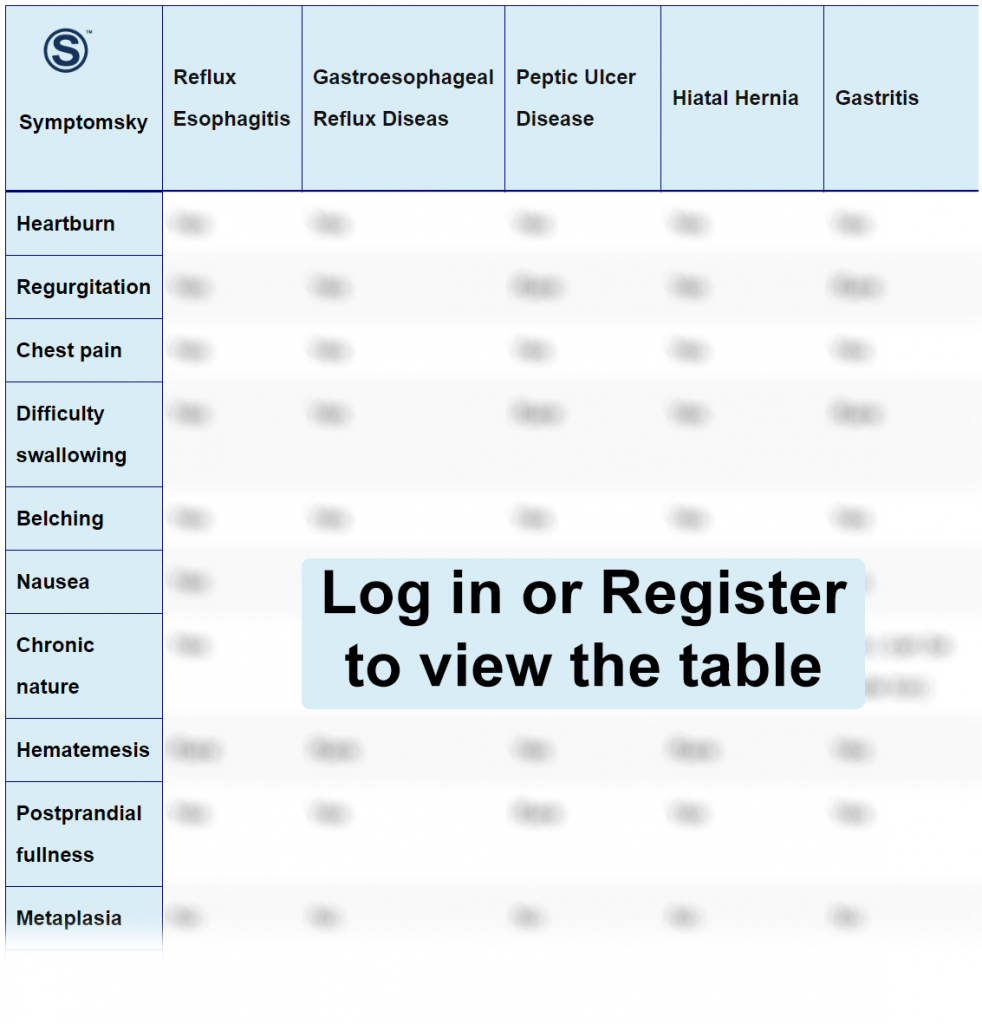
- 1 Reflux Esophagitis Differential Diagnosis Table:
- 2 How to Distinguish Reflux Esophagitis from Other Diseases
- 2.1 Distinguish Gastroesophageal Reflux Disease from Reflux Esophagitis – Diagnosis
- 2.2 Distinguish Peptic Ulcer from Reflux Esophagitis – Diagnosis
- 2.3 Distinguish Hiatal Hernia from Reflux Esophagitis – Diagnosis
- 2.4 Distinguish Gastritis from Reflux Esophagitis – Diagnosis
- 2.5 Distinguish Functional Dyspepsia from Reflux Esophagitis – Diagnosis
- 2.6 Distinguish Barrett’s Esophagus from Reflux Esophagitis – Diagnosis
- 2.7 Distinguish Functional Heartburn from Reflux Esophagitis – Diagnosis
- 2.8 Distinguish Esophageal Stricture from Reflux Esophagitis – Diagnosis
- 2.9 Distinguish Eosinophilic Esophagitis from Reflux Esophagitis – Diagnosis
- 3 Important Red Flags in Reflux Esophagitis
Reflux Esophagitis Differential Diagnosis Table:
Esophagitis is an inflammation of the esophagus. This can happen due to several causes. Reflux esophagitis is the most common cause; it happens due to the backflow of stomach content into the esophagus. This leads to symptoms of heartburn, chest pain, and difficulty swallowing.
Reflux esophagitis mainly happens due to a problem in the valve (Lower esophageal sphincter) that is responsible for preventing ingested food and acids in the stomach from going up into the esophagus. When this valve fails to close properly, this may lead to the reflux of stomach content, leading to esophagitis.
Reflux esophagitis is usually a chronic condition, but medication can help in managing symptoms and improving the quality of life.
Endoscopy is the main diagnostic test for esophagitis, in which the doctor will be able to see any abnormality or inflammation in the esophagus tissue.
How to Distinguish Reflux Esophagitis from Other Diseases
Distinguish Gastroesophageal Reflux Disease from Reflux Esophagitis – Diagnosis
Gastroesophageal reflux disease (GERD) is a very common disease affecting most elderly people, especially. When stomach content moves upward, causing inflammation of the esophagus and in severe cases may lead to damage and inflammation in the pharynx and respiratory tract too, causing throat pain.
- Upper endoscopy is the initial diagnostic test in GERD, although a small percentage of people will have normal findings, but it’s important to rule out any abnormality or complication that may occur.
- Barium esophagram is a very common procedure for the diagnosis of GERD, in which the patient will swallow barium, and X-ray imaging test will be done; this will help to show any presence of esophagus stricture or narrowing.
- Esophageal PH testing or Reflux testing, through an endoscope, the doctor will place a chip for 24 hours to evaluate PH inside the esophagus.
- Esophageal manometry can help in ruling out other conditions, but it’s not useful in the diagnosis of GERD itself.
“Diagnosis of GERD can happen mainly through physical examination and history; more often, doctors will begin treatment immediately if typical symptoms of heartburn and regurgitation are present.”
Distinguish Peptic Ulcer from Reflux Esophagitis – Diagnosis
Peptic ulcer is a sore in the lining of the stomach or intestine; this leads to burning pain in the stomach, and sometimes it progresses to perforation that may cause back pain. Peptic ulcer has three common types: NSAID-induced ulcer, H. pylori-induced ulcer, or stress-induced ulcer.
- Upper endoscope can help in the diagnosis of peptic ulcer, for visualization of intestine lining and the presence of ulcers and perforation.
- H. pylori testing like stool antigen test is important since one of the most common causes of peptic ulcer is H. pylori.
- Upper gastrointestinal series in which the patient swallows barium, and a series of x-ray images are taken; this helps in the diagnosis since ulcers become more visualized.
Distinguish Hiatal Hernia from Reflux Esophagitis – Diagnosis
Hiatal hernia is a condition where a part of the stomach bulges through the diaphragm. This is a very common condition in older people. Although hiatal hernia can be completely asymptomatic, in some cases, it causes symptoms of acid reflux, heartburn, and chest pain.
- Upper endoscope for visualization of the stomach and esophagus will show stomach herniation.
- An upper gastrointestinal series or barium swallow to help take x-ray images and take a better look at the stomach and intestine.
- Since the first symptoms of hiatal hernia are acid reflux, the doctor may initiate the diagnosis with esophageal pH testing and follow up with other imaging tests.
- Chest X-ray maybe useful too in diagnosis and a non-invasive method for the diagnosis of hernia.
Distinguish Gastritis from Reflux Esophagitis – Diagnosis
Gastritis is an inflammation in the lining of the stomach; this leads to stomach pain, nausea, and a feeling of fullness. Usually, gastritis is very common and can happen from various reasons, including certain foods, alcohol, infections (bacterial or viral), or drugs. Gastritis can either be acute or chronic.
- Gastritis can be confirmed by an upper endoscope; the doctor will be able to diagnose gastritis by visualization, but a biopsy may be needed for further confirmation.
- Upper gastrointestinal series or barium swallow, where a series of x-ray images are taken, can help to identify gastritis and rule out any complications or causes.
- H. pylori tests like stool antigen tests are routinely made since H. pylori often causes gastritis and stomach pain as well.
Distinguish Functional Dyspepsia from Reflux Esophagitis – Diagnosis
Functional dyspepsia is a chronic condition of stomach indigestion; it causes symptoms like that of a peptic ulcer: stomach pain or discomfort, nausea, and a feeling of fullness. The exact cause of functional dyspepsia is unknown, and most diagnostic tests will be normal.
Since functional dyspepsia doesn’t have an apparent cause, diagnostic tests will be done to exclude other conditions.
- Upper endoscope will be done to show any structural problems or inflammation present in the stomach and intestine.
- Upper gastrointestinal series with barium swallow to give several X-ray images that can help doctors see if there’s any structural problem present.
- H. pylori tests like stool antigen tests and urea breath tests must be done since H. pylori can cause dyspepsia.
“If all these tests are negative and didn’t show any problems, and the patient has these symptoms for more than 3 months, then the patient is diagnosed with functional dyspepsia.”
Distinguish Barrett’s Esophagus from Reflux Esophagitis – Diagnosis
Barrett’s esophagus is a condition that occurs from long-term acid reflux in the esophagus, which leads to inflammation and damage in esophagus tissues, leading to a change in cells. If progressed, Barrett’s esophagus can lead to esophageal cancer.
- Upper endoscope is generally used for diagnosis, where the esophagus will appear pink or red and velvety.
- After endoscope, a tissue biopsy may be needed to determine the degree of tissue damage and dysplasia. (No dysplasia, low-grade dysplasia, and high-grade dysplasia)
- Chromonendoscopy is a method where during endoscope, a stain is produced to identify normal cells from malignant or cancerous cells in the esophagus.
Distinguish Functional Heartburn from Reflux Esophagitis – Diagnosis
Functional heartburn is a GERD-like symptom condition; it causes the same heartburn in the epigastric area and extends retrosternal, but functional heartburn doesn’t have an exact cause, there are no structural or physiological abnormalities.
- Upper endoscope to exclude any esophageal narrowing or stomach problem; like hiatal hernia.
- 24-hour pH manometry testing to see acid reflux in the esophagus. In the absence of acid reflux with the presence of heartburn symptoms to exclude GERD.
- Esophageal manometry to see any abnormalities in esophagus pressure and esophageal motility. (must be free)
“Diagnosis of functional heartburn depends on the absence of any structural or physiological problems with heartburn that is refractory to PPI treatment.”
Distinguish Esophageal Stricture from Reflux Esophagitis – Diagnosis
Esophageal stricture is narrowing or tightening in the esophagus; this leads to dysphagia, a burning sensation in the throat, and sometimes can lead to stridor. Esophageal stricture can be cancerous or benign. A lot of conditions can cause esophageal stricture such as GERD, peptic ulcer, cancer, or previous surgery.
- Upper endoscope can diagnose and visualize narrowing in the esophagus, and if necessary, a biopsy may be taken if malignancy is suspected.
- Imaging tests like ultrasound can show how much narrowing in the esophagus has occurred.
- Barium swallow with X-ray gives detailed images of the esophagus.
Distinguish Eosinophilic Esophagitis from Reflux Esophagitis – Diagnosis
Eosinophilic esophagitis is a condition in which there’s eosinophils present in the esophagus (Normally esophagus is free from eosinophils); eosinophils are immune cells, they cause inflammation in the esophagus and maybe narrowing. This leads to symptoms of dysphagia and heartburn.
- An upper endoscope with biopsy can confirm eosinophilic esophagitis by the presence of eosinophilic infiltration.
- A barium swallow test may show circular rings, esophageal narrowing, or strictures.
- Patch testing can be done to identify the triggers or allergens.
Important Red Flags in Reflux Esophagitis
Reflux esophagitis is a very common condition and can be easily managed with treatment, but some alarming symptoms must be kept in consideration.
Difficulty swallowing may be reflecting that the esophagus is narrowing, maybe due to erosion or fibrosis, which may indicate a complication from the disease itself or another condition.
Vomiting of blood is very rare to occur with reflux esophagitis but if present may indicate a perforated peptic ulcer which may require surgery.
A very common alarming symptom is chest pain since epigastric pain from esophagitis and chest pain from angina are similar; the patient may be confused about the origin of the pain. so it’s important to seek immediate medical attention especially if the chest pain is radiating to the arm or neck.
