Contents
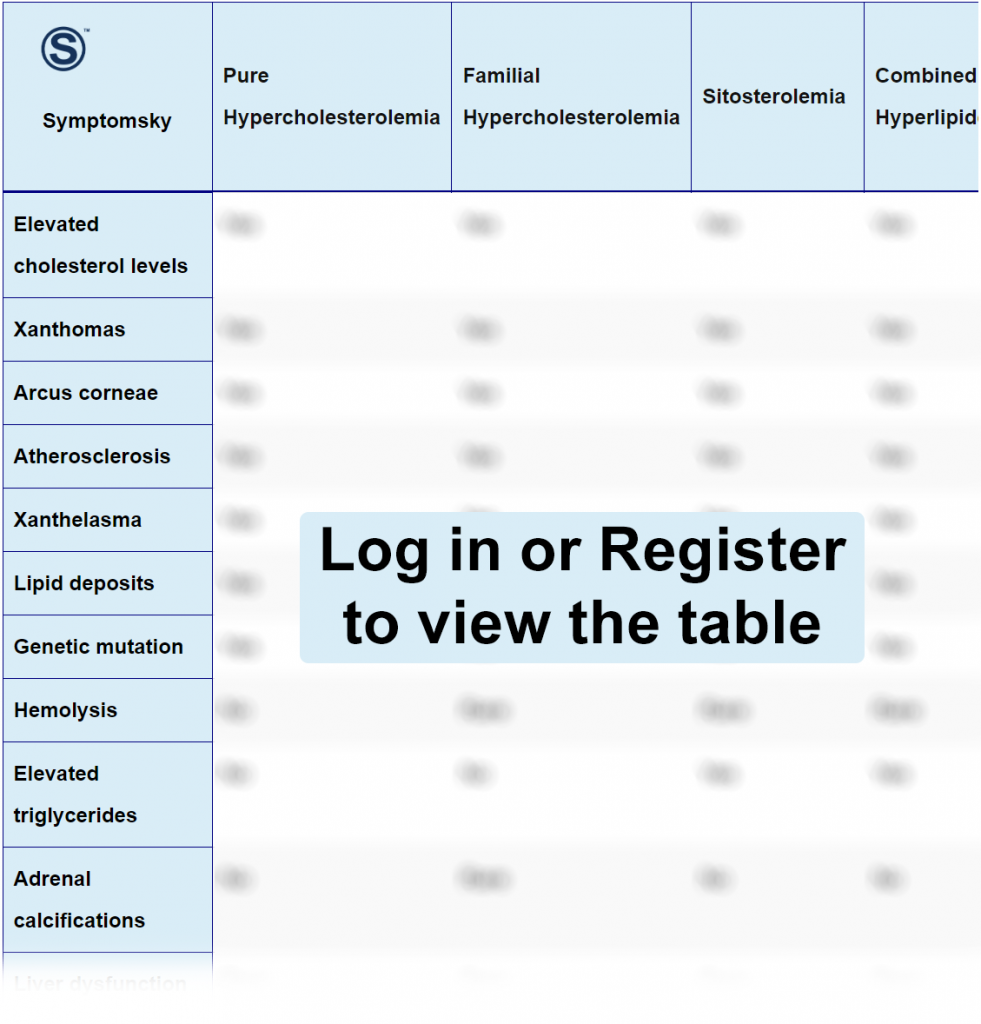
- 1 Pure Hypercholesterolemia Differential Diagnosis Table:
- 2 How To Distinguish Pure Hypercholesterolemia from Other Diseases
- 2.1 Distinguish Familial Hypercholesterolemia from Pure Hypercholesterolemia – Diagnosis
- 2.2 Distinguish Sitosterolemia from Pure Hypercholesterolemia – Diagnosis
- 2.3 Distinguish Combined Hyperlipidemia from Pure Hypercholesterolemia – Diagnosis
- 2.4 Distinguish Cholesteryl Ester Storage Disease from Pure Hypercholesterolemia – Diagnosis
- 2.5 Distinguish Primary Biliary Cirrhosis from Pure Hypercholesterolemia – Diagnosis
- 2.6 Distinguish Tangier Disease from Pure Hypercholesterolemia – Diagnosis
- 2.7 Distinguish Apolipoprotein B Deficiency from Pure Hypercholesterolemia – Diagnosis
- 2.8 Distinguish Abetalipoproteinemia from Pure Hypercholesterolemia – Diagnosis
- 2.9 Distinguish Phytosterolemia from Pure Hypercholesterolemia – Diagnosis
- 3 Important Red Flags in Pure Hypercholesterolemia
Pure Hypercholesterolemia Differential Diagnosis Table:
Pure hypercholesterolemia is a disorder that causes a very high level of LDL, which we call the bad cholesterol. With an increase of LDL in the body, it becomes more susceptible to lipid deposits and the formation of atherosclerosis, which eventually will lead to coronary heart disease.
Most patients with pure or primary hypercholesterolemia don’t know they have the disease until the symptoms of the first coronary artery event occur.
Hypercholesterolemia has many causes; maybe genetic, which is very hard to manage through only diet and exercise, or maybe due to obesity and diabetes.
Most people refer to pure hypercholesterolemia as the same as familial hypercholesterolemia.
How To Distinguish Pure Hypercholesterolemia from Other Diseases
Distinguish Familial Hypercholesterolemia from Pure Hypercholesterolemia – Diagnosis
Familial hypercholesterolemia is a genetic disorder that causes an increase in LDL and total cholesterol levels in the body, leading to many heart problems. In familial hypercholesterolemia, it’s very hard to manage lab levels of High LDL, and medical treatment is usually a necessity.
- Genetic testing in LDLR, APOB, and PCSK9 genes can confirm the diagnosis of familial hypercholesterolemia.
- Blood tests that show high LDL, total cholesterol, and normal triglycerides can help in diagnosis too.
“A family history is very important in confirmation of disease, especially if the disease came from both parents, which is very rare.”
Distinguish Sitosterolemia from Pure Hypercholesterolemia – Diagnosis
Sitosterolemia is a rare genetic disorder caused by a mutation in genes ABCG5 or ABCG8. It causes the body to store plant sterols that come from foods like nuts and plants, causing them to build up instead of excreting them through the stomach. This too leads to atherosclerosis and coronary heart diseases.
- Measuring serum levels of plant sterols is the most diagnostic test for sitosterolemia.
- Detecting gene mutations in the causative genes ABCG5 and ABCG8 can confirm the genetic disorder and diagnosis as well.
“Diagnosis of sitosterolemia is usually not easy due to the resemblance of symptoms to other conditions causing high cholesterol levels and lack of awareness about the disease as well.”
Distinguish Combined Hyperlipidemia from Pure Hypercholesterolemia – Diagnosis
Combined Hyperlipidemia is a disorder causing increased cholesterol, triglycerides, LDL, and a decrease in HDL. This condition is usually genetic, but sometimes it can occur due to other diseases like diabetes or obesity. There’s a high risk for atherosclerosis and coronary heart diseases as well.
- Diagnosis of combined hyperlipidemia mainly depends on a lipid panel showing; high Cholesterol, triglycerides, LDL, and apolipoprotein IIIB.
“Combined hyperlipidemia is a very complex disease to diagnose due to variability of conditions that can cause an increase in the same tests, there are a lot of current research about this condition.”
Distinguish Cholesteryl Ester Storage Disease from Pure Hypercholesterolemia – Diagnosis
Cholesteryl ester storage disease is a rare genetic disorder caused by lysosomal acid lipase (LAL) deficiency, leading to accumulation of cholesteryl and triglycerides in tissue, leading in most cases to hepatomegaly and liver dysfunction. Eventually, patients may need a liver transplant.
- Measuring LAL activity in leukocytes in a blood sample is the most diagnostic test.
- Genetic testing to detect a mutation in the LAL gene.
“Clinical presentation of hepatomegaly along with an increase in lipid panel is usually very diagnostic for this condition.”
Distinguish Primary Biliary Cirrhosis from Pure Hypercholesterolemia – Diagnosis
Primary biliary cirrhosis, known now as Primary biliary cholangitis (PBC), is an autoimmune disorder that causes inflammation of the bile duct and slowly destroys it. This leads to liver injury, liver fibrosis, and eventually cirrhosis, hence the name. Its symptoms are usually the typical symptoms of jaundice alongside fatigue and itching.
- The presence of Antimitochondrial antibodies (AMA) is very characteristic for PBC, being positive in 95% of patients.
- Liver biopsy can help in the confirmation of diagnosis and knowing the depth of liver injury.
“Elevation of gamma-glutamyl transferase and alkaline phosphatase are very indicative too for PBC.”
Distinguish Tangier Disease from Pure Hypercholesterolemia – Diagnosis
Tangier disease is a rare genetic disorder that causes very low HDL in the body, which is the good lipoprotein in your body responsible for removing fats from organs and tissue to the liver. This can lead to coronary heart disease and atherosclerosis. Tangier disease can be asymptomatic until very old age.
- Genetic testing of the ABCA1 gene, which is responsible for the formation of HDL, is diagnostic for this condition.
- A low level of HDL can help confirm the diagnosis.
- Sometimes in people who are unable to do genetic testing, a liver biopsy can be done.
Distinguish Apolipoprotein B Deficiency from Pure Hypercholesterolemia – Diagnosis
Apolipoprotein B deficiency is a genetic disorder that causes a decreasing affinity between apolipoprotein, which is responsible for carrying LDL. Due to this, LDL accumulates in tissue, increasing the likelihood of atherosclerosis and coronary heart diseases. This disease is also known as normotriglyceridemic hypobetalipoproteinemia.
- Apo B test, which is a normal blood test, can count Apolipoprotein B in your body and detect deficiency.
- Genetic testing for Apo B can detect mutations in the gene responsible for the formation of apolipoprotein B.
“Immunonephelometry has also been mentioned a few times as a method that can be used in apolipoprotein assay.”
Distinguish Abetalipoproteinemia from Pure Hypercholesterolemia – Diagnosis
Abetalipoproteinemia is a genetic disorder that causes the failure of absorption of fats in the small intestine due to a mutation in microsomal triglyceride transfer protein. Failure of fat absorption leads to many complications in the nervous system, in muscle strength, and of course, causes many gastrointestinal problems such as steatorrhea and malabsorption.
- Genetic testing for microsomal triglyceride transfer protein is maybe the only test that can confirm this condition.
- A child with an elevated lipid panel and steatorrhea is usually very indicative of this condition in infancy and is the initial step for diagnosis before confirmation by genetic testing.
Distinguish Phytosterolemia from Pure Hypercholesterolemia – Diagnosis
Phytosterolemia, also known as sitosterolemia discussed earlier, is a condition in which the body absorbs too much plant sterol in the diet that leads to accumulation of fat deposits, which increase the risk of coronary artery disease.
- Plant sterol level assay is usually diagnostic for this condition.
- Genetic testing for genes ABCG5 and ABCG8, which are responsible for this condition.
“Elevation in lipid profile such as cholesterol, triglycerides, and LDL are important, since they are usually the first sign of an abnormal condition.”
Important Red Flags in Pure Hypercholesterolemia
High cholesterol level usually goes unnoticed or is asymptomatic. So when experiencing some symptoms, it’s important to seek immediate medical attention.
Chest pain may be an indication of atherosclerosis and coronary artery problems. Another problem that may occur is peripheral artery diseases (PAD), which are common with high cholesterol levels. An unusual sign for PAD is intermittent claudication, which may appear as pain or discomfort in your leg or buttocks.
If you notice the appearance of xanthoma, it means your cholesterol level is alarming since it only occurs in severely progressed hypercholesterolemia.
