Contents
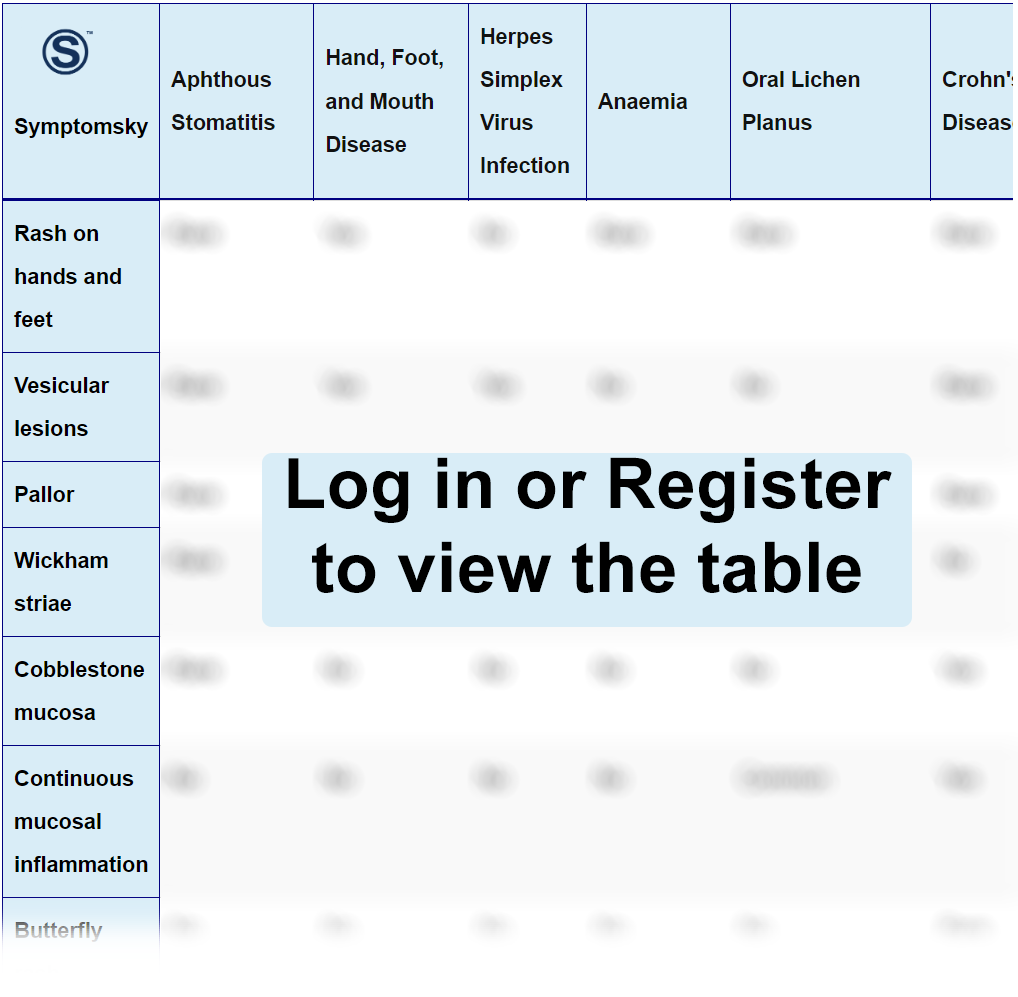
- 1 Oral Ulcer Differential Diagnosis Table:
- 2 How To Recognize Which Disease Is Causing the Oral Ulcer
- 2.1 How to Recognize if Aphthous Stomatitis is Causing Oral Ulcer
- 2.2 How to Recognize if Hand, Foot, and Mouth Disease is Causing Oral Ulcer
- 2.3 How to Recognize if Herpes Simplex Virus Infection is Causing Oral Ulcer
- 2.4 How to Recognize if Anemia is Causing Oral Ulcer
- 2.5 How to Recognize if Oral Lichen Planus is Causing Oral Ulcer
- 2.6 How to Recognize if Crohn’s Disease is Causing Oral Ulcer
- 2.7 How to Recognize if Ulcerative Colitis is Causing Oral Ulcer
- 2.8 How to Recognize if Systemic Lupus Erythematosus is Causing Oral Ulcer
- 2.9 How to Recognize if Behçet’s Disease is Causing Oral Ulcer
- 2.10 How to Recognize if Leukemia is Causing Oral Ulcer
- 2.11 How to Recognize if Oral Tuberculosis is Causing Oral Ulcer
- 2.12 How to Recognize if Oral Squamous Cell Carcinoma (OSCC) is Causing Oral Ulcer
- 3 Common Red Flags With Oral Ulcers
Oral Ulcer Differential Diagnosis Table:
An oral ulcer is a breach in the mucosal lining of the oral cavity. It is tough to pinpoint the exact etiology because aphthous stomatitis has been linked to a number of conditions. The long list of causes includes stress, menstruation, hormonal imbalance, local trauma, smoking, nutritional deficiencies like anemia, leukemia, immunocompromised states like HIV, bacterial, viral, or fungal infections, and as a manifestation of gastrointestinal disorders like celiac disease, ulcerative colitis, and Crohn’s disease. Rarely, they are present as a sign of oral cancer.
Having an oral ulcer is usually an unpleasant experience. People feel an intense pain sensation in the area where the ulceration is present, and it is usually sensitive to hot and spicy foods. The region around the ulcer is red and the center part is yellow to white in color.
Diagnosis is based on history and clinical examination. History should be taken about the time it was first noticed, aggravating factors, relieving factors, and trauma. Clinical examination should be carried out to see if the ulcer is solitary or not, appearance, texture, and extent. If any ulcer is not healing beyond 4 weeks, it is an indication of a biopsy.
How To Recognize Which Disease Is Causing the Oral Ulcer
How to Recognize if Aphthous Stomatitis is Causing Oral Ulcer
Aphthous stomatitis term is made from two words aphthae (ulcer) and stomatitis (inflammation of the mouth). This condition represents itself by small painful ulcers in the oral cavity that usually go back in a week or two on their own. This type of ulceration is usually observed on the non-keratinized mucosa of the oral cavity, which comprises all inside of the cheek and lips, under the surface of the tongue, and the floor of the mouth.
On the clinical examination, aphthous ulcers can be a few mm to a cm in diameter and are usually less in number ranging between 1-10.
How to Recognize if Hand, Foot, and Mouth Disease is Causing Oral Ulcer
Hand, foot, and mouth disease is a viral disease caused by Coxsackie virus. It is a viral infection accompanied by a sense of malaise, weakness, fever, and sore throat. The most distinguishing feature of this disease is that this disease is not only confined to the oral cavity. The ulceration can be observed on the hands and feet as well. Another important sign is that the hand, foot, and mouth disease is contagious.
How to Recognize if Herpes Simplex Virus Infection is Causing Oral Ulcer
Herpes simplex virus infection is another viral infection caused by herpes simplex virus (HSV). HSV has two subtypes, HSV-1 and HSV-2. HSV-1 is usually associated with oral lesions, while HSV-2 is commonly linked with genital herpes. Herpes is a viral infection accompanied by symptoms like fatigue, fever, and general malaise. Oral herpes is mostly on the keratinized mucosa. Herpetic ulceration appears first as a vesicle and then ruptures into an ulcer.
During the clinical examination, herpetic vesicles usually measure less than 1 mm and are multiple, ranging up to 100 in number.
How to Recognize if Anemia is Causing Oral Ulcer
Anemia is a condition in which the number of red blood cells or the hemoglobin is lower than normal. Anemia produces paleness in the skin, fatigue, weakness, and dizziness. Anemia can also cause sore tongue and angular cheilitis. If oral ulcers are due to anemia, these signs will be present along with the ulceration. However, they will be absent if anemia is not present.
How to Recognize if Oral Lichen Planus is Causing Oral Ulcer
Lichen planus is an autoimmune condition that produces mucocutaneous chronic inflammation. It can be present in 5 types. The type producing most of the ulceration is erosive.
The most distinguishing feature of lichen planus is the presence of a white lace-like pattern on the buccal mucosa known as “Wickham Striae”. Moreover, most of the diseases producing oral ulceration cause unilateral ulcers, but lichen planus usually presents itself bilaterally and is usually symmetrical.
Another unique feature is that they can be present on the genital region as well. Furthermore, lichen planus is a chronic condition that stays for months, while most of the oral ulcers heal in 10-14 days.
How to Recognize if Crohn’s Disease is Causing Oral Ulcer
Crohn’s disease is a chronic inflammatory condition of the digestive tract. Crohn’s disease produces oral symptoms like oral ulceration, angular cheilitis, and gum swelling. The most characteristic feature of Crohn’s disease is “cobblestone mucosa”. Other than that, these patients always have a history of abdominal pain and diarrhea.
How to Recognize if Ulcerative Colitis is Causing Oral Ulcer
Ulcerative colitis (UC) is a chronic inflammatory condition of the large intestine only. Ulcerative colitis is also a part of inflammatory bowel disease along with Crohn’s disease.
Patients with ulcerative colitis suffer from diarrhea and stomach pain. Ulcerative colitis also produces oral ulceration and other signs like atrophic tongue, burning mouth, and halitosis. Some studies suggest that ulcerative colitis may cause periodontitis.
How to Recognize if Systemic Lupus Erythematosus is Causing Oral Ulcer
Systemic lupus erythematosus is an autoimmune condition that affects organs all over the body. The most striking feature of the disease is the presence of a very characteristic rash on the face known as “butterfly rash”. Lupus results in inflammation throughout the body, so its symptoms are spread all over the body. So, the symptoms are not only limited to the mouth. In lupus, along with oral ulceration, people feel pain in their joints from arthritis.
How to Recognize if Behçet’s Disease is Causing Oral Ulcer
Behçet’s disease is a condition that causes inflammation in the blood vessels of the body. In Behçet’s disease, genital ulceration will be present along with oral ulceration. Behçet’s disease produces intense ocular symptoms, starting from blurry vision and teary eyes, leading to vision loss.
How to Recognize if Leukemia is Causing Oral Ulcer
Leukemia is a malignancy of the blood cells. Leukemia patients bleed more easily. Spontaneous hemorrhage results in signs of weakness, fatigue, and paleness. Along with ulceration, these patients have gingiva that bleeds spontaneously. Other than that, gingival hyperplasia is a very common feature of leukemia. Petechial hemorrhage is another common sign of leukemia.
How to Recognize if Oral Tuberculosis is Causing Oral Ulcer
Tuberculosis is an infectious disease caused by bacteria that usually affects the lungs. However, it can affect other parts of the body as well, especially the oral cavity where it can produce ulceration. TB usually affects the tongue with a non-healing painless ulcer. With TB, it is common to have regional lymphadenopathy.
How to Recognize if Oral Squamous Cell Carcinoma (OSCC) is Causing Oral Ulcer
Oral squamous cell carcinoma (OSCC) refers to the malignant transformation of cells present at the junction of the hard and soft palate, tongue, floor of the mouth, and the vermilion border of the lip.
Most of the ulcerations associated with OSCC aren’t painful. They can be differentiated from other diseases by the duration. Any ulcer persisting for more than 4 weeks is suspected of malignancy. Other than that, oral malignancy ulcers are usually indurated with hard borders on palpation.
There may be other signs of malignancy present along with ulceration like enlarged lymph nodes, dysphagia, and dysphonia. These are never present with other diseases.
Common Red Flags With Oral Ulcers
Oral ulceration is a very mild disease yet very painful. The most common reason producing these can be stress, even from exams. There is nothing to be concerned about as they resolve in 7-10 days. When they don’t resolve in 4 weeks, it is a matter of concern. Any oral ulceration persisting more than 3 weeks should be referred for biopsy.
The most important red flag with oral ulceration is a non-healing ulcer with marked, rolled, and hard borders. Other signs include symptoms not associated with ulceration like lymphadenopathy, fatigue, malaise, fever, diarrhea, abdominal pain, and spontaneous bleeding. Such lesions should always be biopsied to rule out the presence of malignancy.
