Contents
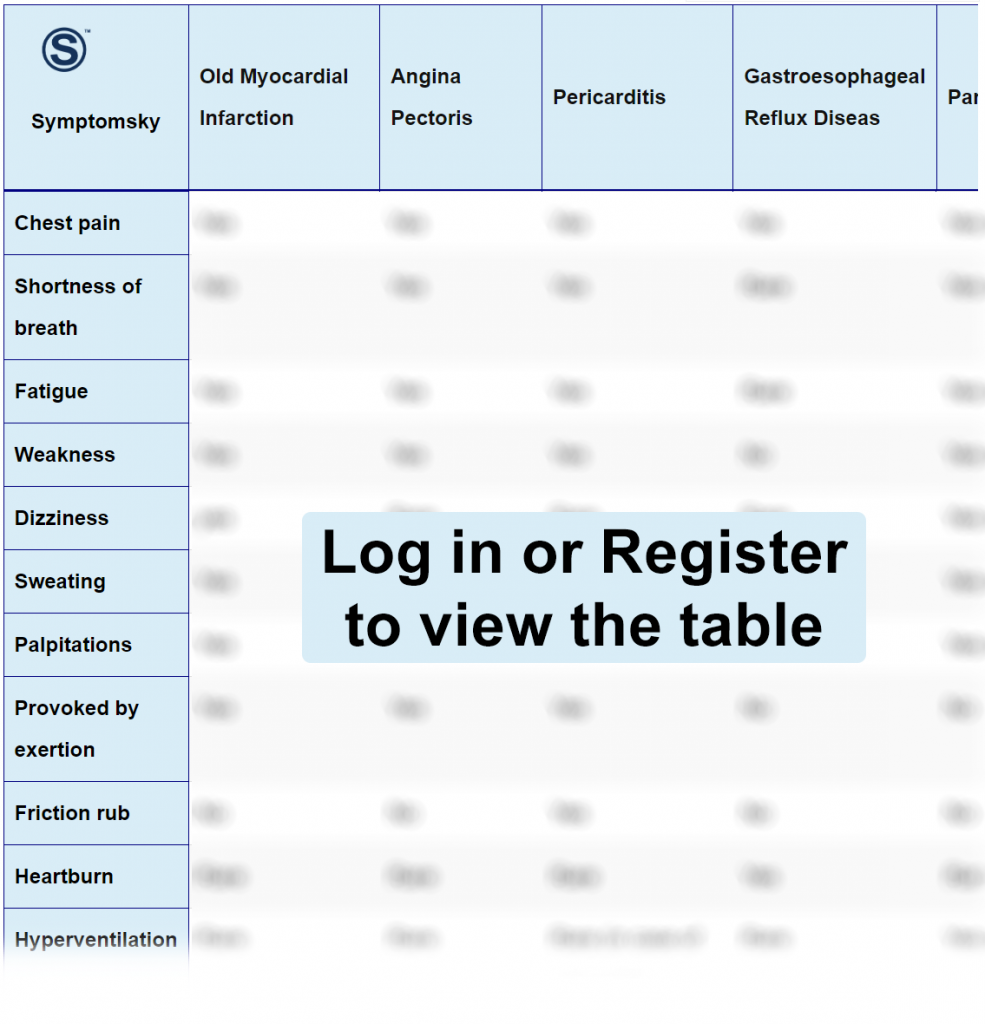
- 1 Old Myocardial Infarction Differential Diagnosis Table:
- 2 How to Distinguish Myocardial Infarction from Other Diseases
- 2.1 Distinguish Angina Pectoris from Myocardial Infarction – Diagnosis
- 2.2 Distinguish Pericarditis from Myocardial Infarction – Diagnosis
- 2.3 Distinguish Gastroesophageal Reflux Disease from Myocardial Infarction – Diagnosis
- 2.4 Distinguish Panic Attacks from Myocardial Infarction – Diagnosis
- 2.5 Distinguish Costochondritis from Myocardial Infarction – Diagnosis
- 2.6 Distinguish Aortic Stenosis from Myocardial Infarction – Diagnosis
- 2.7 Distinguish Hypertrophic Cardiomyopathy from Myocardial Infarction – Diagnosis
- 2.8 Distinguish Pulmonary Embolism from Myocardial Infarction – Diagnosis
- 2.9 Distinguish Pleuritis from Myocardial Infarction – Diagnosis
- 3 Important Red Flags in Old Myocardial Infarction
Old Myocardial Infarction Differential Diagnosis Table:
A myocardial infarction, also commonly referred to as a heart attack, is the death of heart cells due to a lack of oxygen supply to the heart for a period of time, usually 30 minutes or more.
Myocardial infarction is a life-threatening condition that requires immediate medical treatment. Sometimes myocardial infarction can go unnoticed, which is more common in women and more dangerous since the patient doesn’t receive adequate medical treatment, which may lead to a bad prognosis.
Most often, myocardial infarction is caused by increased fats in the body that lead to atherosclerosis and fat plaques that may travel through the blood and block blood supply to the heart.
Initial steps for the diagnosis of myocardial infarction are by diagnostic markers like troponin (stays more in the blood, so can detect old myocardial infarction) and creatine kinase. Further diagnostic tests like ECG and echo are necessary for confirmative diagnosis as well.
How to Distinguish Myocardial Infarction from Other Diseases
Distinguish Angina Pectoris from Myocardial Infarction – Diagnosis
Angina is a type of coronary artery disease, it’s when the blood supply starts to decrease to the heart maybe due to coronary artery spasm. Angina is a wide term that refers to three types of angina: unstable angina which is the less severe and usually goes on its own with rest, NSTEMI and STEMI.
- ECG can differentiate the three forms of angina with NSTEMI, there’s an ST segment depression, while in myocardial infarction, there’s an ST segment elevation. In unstable angina, there’s an ST segment depression as well (but cardiac markers are negative).
- Cardiac enzymes like troponin and CK will be negative in unstable angina and positive in myocardial infarction.
- Echo can help detect any problems with blood flow to the heart.
- Stress test makes the diagnosis of angina easier, since oxygen demands increase during exercise, it’s usually done along with other tests to facilitate diagnosis.
- Coronary angiography helps show blood vessels inside the heart, it’s a procedure where a catheter is inserted through the heart with a dye to visualize vessels inside the heart.
Distinguish Pericarditis from Myocardial Infarction – Diagnosis
Pericarditis is an inflammation of the cardiac layer; pericardium that can cause symptoms of chest pain and fatigue. It usually happens due to a virus or bacterial infection and can be managed with medical treatment and antibiotics, but if left untreated can lead to complications like increased or enlarged heart thickness.
- ECG can diagnose pericarditis; it shows a characteristic concave ST elevation and PR depression, although stages of pericarditis affect how it looks on ECG.
- Echo can show signs of pericardium thickening and enlargement and can help show if the disease has progressed to pericardial effusion.
- CT scan and cardiac MRI can visualize any inflammation or change in the pericardium.
- Routine blood tests like CRP, ESR, and CBC can help in prognosis and monitor of infection and are usually used routinely to see effectiveness of treatment as well.
Distinguish Gastroesophageal Reflux Disease from Myocardial Infarction – Diagnosis
Gastroesophageal reflux disease (GERD) is a condition in which stomach contents move upward to the esophagus and maybe to the pharynx and throat, causing heartburn and difficulty swallowing. This usually happens due to a problem in the lower esophageal sphincter where it can’t completely close after digestion making food move upward to the esophagus.
- Upper endoscopy can be helpful in identifying any damage that happens to the esophagus due to acid reflux.
- Esophageal manometry can be used to assess contractility and function of muscle and lower esophageal sphincter.
- A wireless pH monitoring is one of the most diagnostic tests for GERD; a probe is inserted into the patient’s esophagus and monitors the acid reflux for 48 hours.
- An x-ray of the esophagus (esophagram) with barium contrast can help detect any damage to the esophagus and detect any abnormalities during swallowing.
“Sometimes the symptoms of the chest pain in GERD resemble those of myocardial infarction and a lot of people may mistake myocardial infarction as GERD but there are alarming symptoms that most people need to know to differentiate between both conditions.”
Distinguish Panic Attacks from Myocardial Infarction – Diagnosis
Panic attacks are episodes of fear and anxiety that can happen due to stressful events; sometimes they might occur on their own. They cause symptoms of chest pain, increasing heart rate, and shortness of breath. They give the patient a feeling of danger and although they might cause actual physical harm, they affect quality of life and if they occur so much, the patient might need medical treatment.
Since panic attacks don’t cause actual physical harm, there’s no specific test for diagnosis, but some criteria have been developed to help in diagnosis.
- The criteria of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) is used most by doctors for confirming diagnosis.
- Panic Disorder Severity Scale (PDSS) is also used to assess and measure severity of symptoms.
Distinguish Costochondritis from Myocardial Infarction – Diagnosis
Costochondritis is an inflammation of cartilage that connects ribs to sternum; it can cause symptoms like sharp chest pain that may mimic myocardial infarction, but costochondritis is not a life-threatening condition and usually managed by medical treatment.
Costochondritis doesn’t have a specific diagnostic test and diagnosis is usually based on exclusion of other conditions.
- Blood tests and inflammatory markers like CRP can help in detecting presence of inflammation or infection.
- Imaging tests like X-ray and echo are used to rule out other conditions.
- Physical examination by doctor to assess presence of localized pain.
Distinguish Aortic Stenosis from Myocardial Infarction – Diagnosis
Aortic stenosis is a condition in which the aortic artery that is responsible for delivering blood from the heart to the body starts to get narrow, affecting heart condition. This may lead to bad prognosis, and most people don’t start to feel symptoms until the disease progresses.
- An echo, especially transesophageal echocardiogram (TEE), is the definitive diagnostic test, can help in detecting the severity of aortic stenosis since it helps identify blood flow through the heart.
- Chest x-ray can show images of stenosis of the aorta and see any heart enlargement that may occur as a complication from the disease. This may be done alongside cardiac CT scan.
- ECG can also be used, but it’s not reliable in diagnosing aortic stenosis and results may vary from one patient to another.
Distinguish Hypertrophic Cardiomyopathy from Myocardial Infarction – Diagnosis
Hypertrophic cardiomyopathy is a condition in which heart walls become thickened leading to enlarged heart muscle. This can reduce the ability of the heart to be filled with sufficient blood and its ability to contract to pump blood to the heart. This condition can be genetic but can also occur due to some complications of other heart conditions.
- Echo can be used to assess hypertrophy and thickened heart muscle; it will help know if there’s any obstruction in blood flow through the heart.
- ECG can show characteristic features of cardiomyopathy as “dagger-like” Q waves.
- Cardiac MRI can help visualize thickening of heart wall and enlargement of muscle.
Distinguish Pulmonary Embolism from Myocardial Infarction – Diagnosis
Pulmonary embolism (PE) is a clot in the lung; it usually arises from a blood clot that formed in the body, most commonly in the leg, traveled through the body into the lung. This leads to inability to breathe well, shortness of breath, and decrease in oxygen saturation which is the most common and first sign.
- Chest X-ray is usually the fastest and easiest step for diagnosis of patients with suspected pulmonary embolism.
- Other imaging tests like CT with contrast and MRI can visualize blood vessels and detect pulmonary embolism as well.
- Blood tests like D-dimer increase with thrombosis and pulmonary embolism can help to monitor treatment efficacy.
Distinguish Pleuritis from Myocardial Infarction – Diagnosis
Pleuritis is an inflammation of pleura (which is lining of lung that separates it from the chest wall); when this lining becomes inflamed, that can affect lung capacity to expand leading to sharp chest pain and shortness of breath.
- Imaging tests like CT chest and chest X-ray can show if there’s inflammation in pleura or presence of pleural effusion.
- Thoracentesis: a process in which the doctor uses a needle to remove fluid in pleura for analysis to look for infection or other causes of pleuritis.
- A simple physical examination by a stethoscope where the doctor can hear the friction of pleura together.
Important Red Flags in Old Myocardial Infarction
Myocardial infarction is a life-threatening condition that requires immediate medical attention, although symptoms might go unnoticed but certain red flags present in that disease that require emergency treatment.
Presence of a sudden onset chest pain that radiates to the jaw or left arm, if the patient has this symptom, they need to go to the hospital immediately.
Presence of shortness of breath with vital abnormalities like tachy or bradycardia may indicate there’s a severe blockage in the blood vessel of the heart that blocks blood flow.
Leg swelling if occurred with presence of cardiac disorder or an old myocardial infarction may indicate that heart function is declined that may lead to edema and leg swelling.
