Contents
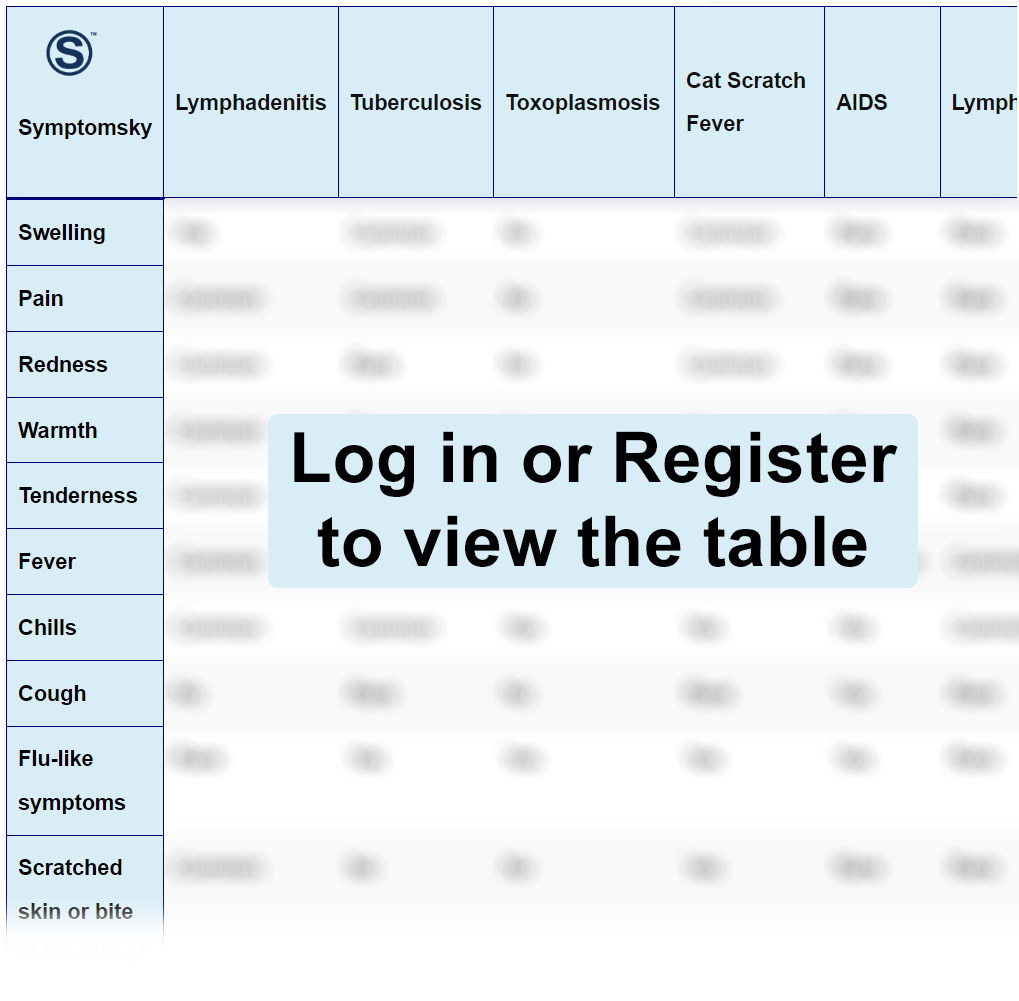
- 1 Lymphadenitis Differential Diagnosis Table:
- 2 How To Distinguish Lymphadenitis From Other Diseases
- 2.1 Distinguish Lymphadenitis from Tuberculosis – Diagnosis
- 2.2 Distinguish Lymphadenitis from Toxoplasmosis – Diagnosis
- 2.3 Distinguish Lymphadenitis from Cat Scratch Fever – Diagnosis
- 2.4 Distinguish Lymphadenitis from AIDS – Diagnosis
- 2.5 Distinguish Lymphadenitis from Lymphoma – Diagnosis
- 2.6 Distinguish Lymphadenitis from Leukemia – Diagnosis
- 2.7 Distinguish Lymphadenitis from Metastatic Breast Cancer – Diagnosis
- 2.8 Distinguish Lymphadenitis from SLE – Diagnosis
- 2.9 Distinguish Lymphadenitis from RA – Diagnosis
- 2.10 Distinguish Lymphadenitis from Kaposi Sarcoma – Diagnosis
- 3 Common Red Flags With Lymphadenitis
Lymphadenitis Differential Diagnosis Table:
To fight foreign threats, the body’s immune system has lymph nodes that act as filters. They contain specialized cells to destroy infectious agents, foreign bodies, damaged cells, and cancerous cells.
Lymphadenitis is an inflammation of the lymph nodes caused by bacterial, viral, or fungal infection anywhere in the body. Lymphadenitis can either be generalized or localized to a specific area of the body.
Swollen lymph nodes are a sign almost always present. Other common symptoms include redness, warmth, pain, and tenderness. Fever and chills can also be present.
How To Distinguish Lymphadenitis From Other Diseases
Distinguish Lymphadenitis from Tuberculosis – Diagnosis
Tuberculosis (TB) is a chronic bacterial infection that predominantly affects the lungs. Non-pulmonary tuberculosis also exists, and it can affect and produce symptoms in the lymph nodes, which can look like lymphadenitis.
- Tuberculosis lymphadenopathy produces symptoms like night sweats and weight loss. These are not common with lymphadenitis.
- A history of an encounter or a family member who is diagnosed with TB is highly suggestive that lymph node swelling is linked to tuberculosis.
- In rare instances, tuberculosis lymphadenopathy can develop into a fistula. It never occurs in lymphadenitis.
“FNAC is a diagnostic test that distinguishes the two.”
Distinguish Lymphadenitis from Toxoplasmosis – Diagnosis
Toxoplasmosis is a parasitic infection that usually produces symptoms in immunocompromised individuals.
- The lymphadenopathy associated with toxoplasmosis is usually asymptomatic, while lymphadenitis frequently produces swelling, redness, and tenderness in the associated region.
- Toxoplasmosis, in some cases, produces ocular symptoms that cause blurred vision, typically feels like looking at a headlight in fog. This is not present in lymphadenitis.
- Toxoplasmosis also produces maculopapular rashes, which are not common in lymphadenitis.
“Detection of the parasite Toxoplasma gondii in polymerase chain reaction confirms toxoplasmosis, which won’t be detected in lymphadenitis.”
Distinguish Lymphadenitis from Cat Scratch Fever – Diagnosis
Cat scratch fever or disease is a bacterial infection spread by a cat’s bite, scratch, or licking over an open wound. It usually produces lymphadenitis.
- With cat scratch fever, there is always a history of an encounter with a cat; this is not always the case with lymphadenitis.
- Unlike lymphadenitis, there is always an erythematous papule or vesicle present at the site of a scratch or bite in cat scratch disease.
- The ocular manifestations of cat scratch disease include conjunctival ulceration and granuloma formation, which turns the eye red-colored. This is not present in lymphadenitis.
“Detection of bacteria Bartonella henselae in polymerase chain reaction confirms cat scratch disease, which won’t be detected in lymphadenitis.”
Distinguish Lymphadenitis from AIDS – Diagnosis
AIDS, or acquired immunodeficiency virus, is a group of symptoms that present due to viral infection caused by HIV.
- The lymphadenopathy associated with AIDS is mostly generalized all over the body rather than being localized to a region in lymphadenitis.
- AIDS patients frequently complain about night sweats, which are uncommon in lymphadenitis.
- Inflammation and pain in joints are common in AIDS; however, it is rare in lymphadenitis.
Distinguish Lymphadenitis from Lymphoma – Diagnosis
Lymphoma is malignant transformation of cells of the lymphatic system.
- Lymphadenitis: Swollen lymph nodes get better within two to three weeks. Lymphadema associated with lymphoma doesn’t get better within this time period.
- The swollen lymph nodes associated with lymphoma are usually painless. In lymphadenitis, they are tender, painful, and appear red.
- Symptoms like night sweats and unexplained weight loss are usually present in lymphoma, not in lymphadenitis.
“On clinical examination, these lymph nodes feel fixed and hard to palpate. While benign lymph node swelling is movable and soft.”
Distinguish Lymphadenitis from Leukemia – Diagnosis
Leukemia is the division of blood cells beyond its limits and produces excessive numbers of abnormal blood cells.
- Lymphadenitis actively produces swelling, redness, tenderness, and pain in the affected lymph node region. It is not common in leukemia-associated lymphadenopathy.
- In leukemia, there is a presence of tiny red, blue, or purple spots known as petechiae on the skin. This never occurs in lymphadenitis.
- Bone pain is a common symptom of leukemia; it is not present in lymphadenitis.
Distinguish Lymphadenitis from Metastatic Breast Cancer – Diagnosis
Metastatic breast cancer is when cancer spreads to another organ of the body.
- In breast cancer, there is an obvious mass in the breast that can be palpable. There is no mass present in lymphadenitis.
- Metastatic breast cancer is an advanced stage of the disease, and in this stage, people usually feel dizziness, visual disturbances, headaches, bone pain, nausea, and vomiting. These signs are not present in lymphadenitis.
- Lymphadenitis usually presents with fever and chills. It is uncommon in breast cancer patients.
Distinguish Lymphadenitis from SLE – Diagnosis
SLE or systemic lupus erythematosus is an autoimmune condition that results in organ damage.
- A very common sign of SLE is a butterfly-shaped rash on the face. This is not present in lymphadenitis.
- SLE patients frequently suffer from joint pain. This is not present in lymphadenitis.
- Patients with SLE often suffer from sicca syndrome, which is the excessive dryness of mucous membranes. Lymphadenitis doesn’t affect the mucous membrane.
Distinguish Lymphadenitis from RA – Diagnosis
RA or rheumatoid arthritis is an inflammatory condition that affects the joints, usually the joints of the extremities. Although it can occur due to a variety of reasons, the most likely cause is autoimmune. Lymph node swelling is a common manifestation in both RA and lymphadenitis.
- In RA, there is always a history of severe pain in joints, stiffness, and swelling. People with lymphadenitis rarely suffer from this.
- In most cases of RA, family history is positive. Lymphadenitis is an infection not linked to genetic etiology.
- Since RA is a chronic inflammatory condition, people usually suffer weight loss. Rare to be associated with lymphadenitis.
“During the clinical examination, RA patients usually show hand signs like Boutonniere deformity, ulnar deviation, and swan-neck deformity of fingers. Other than that, rheumatoid factor test and Anti-Cyclic Citrullinated Peptide (anti-CCP) Antibody Test are positive in RA.”
Distinguish Lymphadenitis from Kaposi Sarcoma – Diagnosis
Kaposi sarcoma is a neoplasm of the skin known to be induced by Human Herpes Virus (HHV8).
- Kaposi sarcoma usually appears as brown, black, or purple-colored skin nodules all over the body. This appearance is characteristic of Kaposi sarcoma and cannot be seen in lymphadenitis.
- Kaposi sarcoma can affect the mucous membranes like the mouth and digestive tract. In this case, it produces bleeding, a rare occurrence in lymphadenitis.
“Biopsy differentiates the two diseases.”
Common Red Flags With Lymphadenitis
Although lymphadenitis is not a serious condition, it is extremely painful. If left untreated, it can develop an abscess or can cause cellulitis, which is life-threatening. Lymph node swelling is a common occurrence in a lot of diseases; however, care should be given to any nodal swelling that is not resolving after 3 to 4 weeks, accompanied by unexplained weight loss, spots or discoloration on the skin, and any palpable mass present in the body. These are the warning signs that should never be ignored.
