Contents
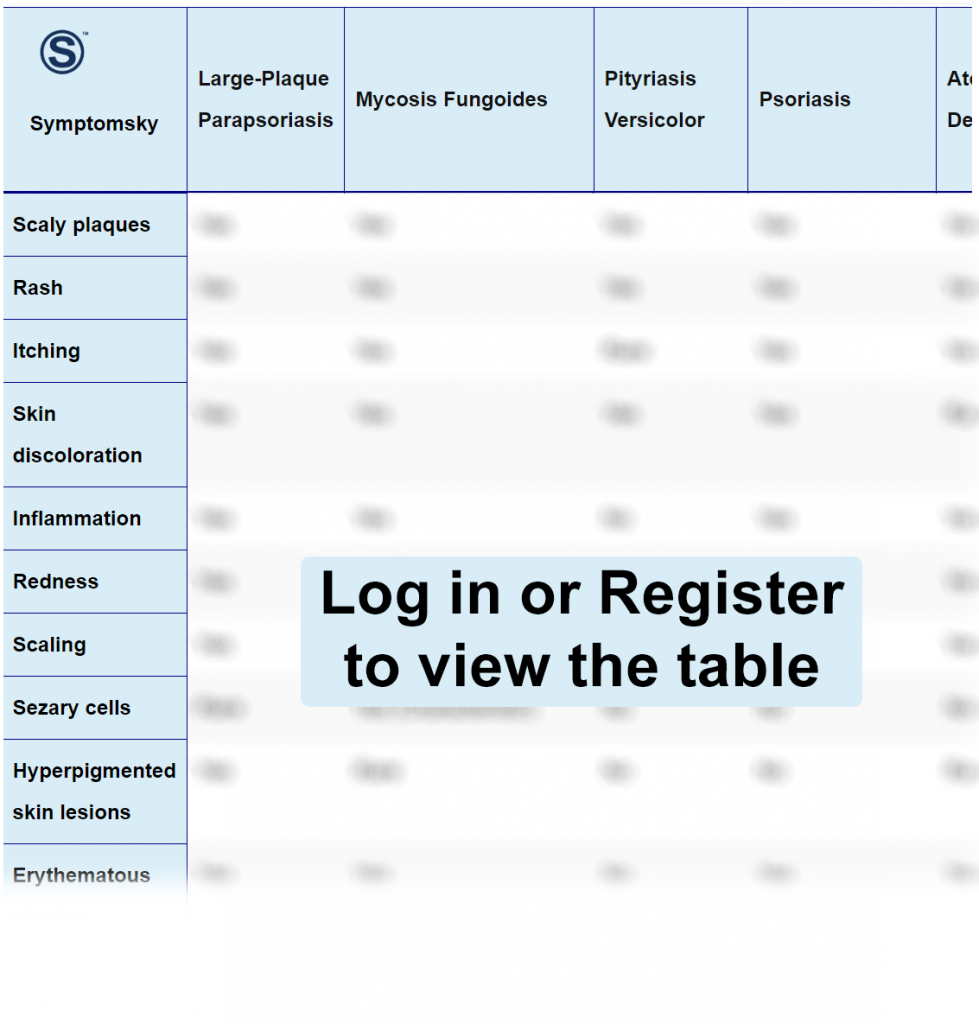
- 1 Large Plaque Parapsoriasis Differential Diagnosis Table:
- 2 How To Distinguish Large Plaque Parapsoriasis from Other Diseases
- 2.1 Distinguish Mycosis Fungoides from Large Plaque Parapsoriasis – Diagnosis
- 2.2 Distinguish Pityriasis Versicolor from Large Plaque Parapsoriasis – Diagnosis
- 2.3 Distinguish Psoriasis from Large Plaque Parapsoriasis – Diagnosis
- 2.4 Distinguish Atopic Dermatitis from Large Plaque Parapsoriasis – Diagnosis
- 2.5 Distinguish Cutaneous T-cell Lymphoma from Large Plaque Parapsoriasis – Diagnosis
- 2.6 Distinguish Eczema from Large Plaque Parapsoriasis – Diagnosis
- 2.7 Distinguish Prurigo Nodularis from Large Plaque Parapsoriasis – Diagnosis
- 2.8 Distinguish Lichen Planus from Large Plaque Parapsoriasis – Diagnosis
- 3 Important Red Flags of Large Plaque Parapsoriasis
Large Plaque Parapsoriasis Differential Diagnosis Table:
Large plaque parapsoriasis is defined as parapsoriasis lesions of more than 5 cm in diameter. It is a chronic, idiopathic, heterogeneous group of inflammatory disorders caused by long-term immunostimulation by an antigen. It appears as irregularly shaped erythematous plaques or papules that are thin, dull, finely scaled, hyperpigmented with superficial wrinkles or atrophy.
The exact cause of this disease is unknown, but it is thought to be caused by T-cell proliferation in the skin. It usually appears in areas that are not directly exposed to the skin, such as the trunk, buttocks, and legs. It can progress into other disorders like cutaneous T-cell lymphoma or Mycosis fungoides.
Diagnosis is mainly made on the clinical examination of the plaques. Treatment options are topical corticosteroids and retinoids; tar and vitamin D analogs can also be used. Light therapy has proven excellent in the treatment of large plaque Parapsoriasis.
How To Distinguish Large Plaque Parapsoriasis from Other Diseases
Distinguish Mycosis Fungoides from Large Plaque Parapsoriasis – Diagnosis
Mycosis Fungoides is a non-treatable type of blood cancer that affects the skin. It is caused by T-cell proliferation. Symptoms include a red rash, which turns into thin eczema-like patches, and then tiny raised papules are formed. The features that distinguish mycosis fungoides from large plaque parapsoriasis are;
- Mycosis fungoides has lymphocytes that reside in the epidermis, while LPP has a thickened epidermis with elongation of rete ridges and focal deposition of lymphocytes and neutrophils.
- Mycosis Fungoides has Sezary cells and enlarged lymph nodes, while LPP rarely has these features.
- Although mycosis fungoides and LPP, due to their clinical similarity, are hard to diagnose, PPP is supposed to be an early expression of mycosis fungoides.
- Skin biopsy is used to distinguish both diseases.
Immunophenotyping and Skin biopsy are used to develop a diagnosis. Treatment options include Radiation therapy, Immunotherapy, Topical corticosteroids, bexarotene, and nitrogen mustard.
Distinguish Pityriasis Versicolor from Large Plaque Parapsoriasis – Diagnosis
Pityriasis Versicolor is caused by overproduction of yeast, which can be normally present on the skin. It appears as small, flat to round patches of skin discoloration that can cause itching and scaling. The features that differentiate pityriasis versicolor from LPP are;
- Pityriasis versicolor is a fungal infection while LPP is caused by the overproliferation of T-lymphocytes.
- Pityriasis versicolor presents as hypopigmented or hyperpigmented finely demarcated patches or papules, while LPP has large, irregular, flat to raised, hyperpigmented papules and patches.
- Pityriasis versicolor shows typical grape-like clusters of yeast cells with long hyphae, while LPP lacks this feature.
- Pityriasis versicolor varies from 1cm to 3cm, while LPP has a size of more than 5cm.
Pityriasis versicolor is diagnosed on clinical examination and examination under UV black light. While to confirm the diagnosis, skin scraping soaked in KOH and examination under a microscope are performed. Antifungal medication is used for treatment.
Distinguish Psoriasis from Large Plaque Parapsoriasis – Diagnosis
Psoriasis is a long-lasting, autoimmune skin disease. It appears as itchy, discolored patches with greyish or silvery-white scales that can appear anywhere in the body, but knees, elbows, lower back, and the scalp are more prone to develop psoriasis. The features which differentiate psoriasis from LPP are;
- Although both have scaly patches, psoriasis patches are thicker than parapsoriasis patches.
- Psoriasis has well-demarcated, pink-colored plaques and papules, while LPP has symptomless, thin, dull, wrinkled, and atrophic patches.
- Psoriasis can occur anywhere but presents significantly on knees, elbows, lower back, and the scalp, while LPP is mostly present on the trunk and often buttocks.
Psoriasis is diagnosed clinically, but skin biopsy can be performed for confirmation of the diagnosis. Treatment options are topical and oral corticosteroids, with phototherapy having proven effective.
Distinguish Atopic Dermatitis from Large Plaque Parapsoriasis – Diagnosis
Atopic Dermatitis or Atopic eczema is a chronic skin condition that causes dryness, intense itching, inflammation, and cracking of the skin. It usually appears in areas of the skin that have the ability to flex or bend. The features which distinguish atopic dermatitis from large plaque parapsoriasis are;
- Atopic Dermatitis is caused by an irritant, stress, infections, and allergens while large plaque parapsoriasis is caused by long-term overstimulation by an antigen.
- Atopic dermatitis is usually found in front of elbows, behind the knees, and neck folds while LPP is usually present on the trunk, thighs, buttocks, and breasts.
- Both diseases can present with an itchy rash, but atopic dermatitis mostly presents in children or the younger age group while LPP is mostly seen in the older age group.
It is diagnosed by looking at the rash, blood tests, and patch tests. It is treated by anti-itch, anti-inflammatory medications, and daily moisturization.
Distinguish Cutaneous T-cell Lymphoma from Large Plaque Parapsoriasis – Diagnosis
Cutaneous T-cell Lymphoma is a rare skin cancer. It is caused when white blood cells, specifically T lymphocytes, abnormally attack skin cells. Symptoms include an itchy rash, red, dry, thick bumps, or raised patches on the skin that are often scaly. The features that differentiate cutaneous T-cell Lymphoma from Large Plaque Parapsoriasis are;
- Cutaneous T-cell lymphoma is usually found in lymph tissues; spleen, bone marrow, tonsils, and skin or peripheral parts of the body like the nose, ear, hands, and feet while large plaque parapsoriasis is found on areas that are not exposed to the sun.
- Moreover, the former shows lymph nodes involvement while the latter doesn’t involve lymph nodes.
- Cutaneous T-cell lymphoma is an aggressive tumor while large plaque parapsoriasis has more than a 90% 5-year survival rate.
- Large Plaque Parapsoriasis is considered to be a precursor of Cutaneous T-cell Lymphoma.
Biopsy is usually done to confirm the diagnosis. Blood tests, examination, and family history are also important. Chemotherapy, radiotherapy, immunosuppressants, Corticosteroids are some of the treatment options.
Distinguish Eczema from Large Plaque Parapsoriasis – Diagnosis
Eczema is a non-contagious skin condition that is caused by a defective skin barrier, resulting in the skin becoming prone to an irritant or an allergen. It causes rashes, itchy, dry skin with scaly patches and blisters that ooze sometimes. The features that distinguish eczema from Large Plaque Parapsoriasis are;
- Eczema is caused by an irritant or an allergen while LPP is caused by the overproduction of T lymphocytes.
- Eczema is present on the cheeks, knees, elbows, hands, and feet while LPP is located on areas that are not directly exposed to the sun.
- Histologically, Eczema has intraepidermal fluid-filled vesicles with exocytosis of lymphocytes present while LPP has dermal lymphocytic infiltrate that may expand into the epidermis.
Eczema is diagnosed on the clinical examination of the lesion, and a patch test can also be performed. Treatment options include; avoidance of an allergen, moisturization, and corticosteroids.
Distinguish Prurigo Nodularis from Large Plaque Parapsoriasis – Diagnosis
Prurigo Nodularis is a long-lasting skin condition caused by excessive scratching, rubbing, and friction on the skin. It appears as raised, thick, intensely itchy lumps and bumps having crust on them. The features that distinguish prurigo nodularis from LPP are;
- Prurigo nodularis develops multiple itching nodules that cause hyperpigmentation or hypopigmentation and may leave scars while LPP can have larger plaques and papules that leave small hyperpigmented scar.
- Prurigo nodularis can be found in people having Dermatitis, Diabetes Mellitus, lymphomas, CKD, and HIV while large plaque parapsoriasis is not associated with these diseases.
- Prurigo nodularis doesn’t have a cure but it is a benign condition while LPP has a tendency to develop in cancer.
It is diagnosed based on the history and examination of bumps, but biopsy and examination under the microscope can also be performed. Anti-itch creams and intralesional steroids can help in relieving the symptoms.
Distinguish Lichen Planus from Large Plaque Parapsoriasis – Diagnosis
Lichen Planus is an immune-related disease of unknown origin. It causes an inflammatory rash on the scalp, oral cavity, arms, legs, genitals, and nails. The features that distinguish lichen planus from Large Plaque Parapsoriasis are;
- Lichen Planus is distinguished from LPP as it has itchy, flat-topped, purple, polygonal plaques and papules which are often covered by white lines called Wickham striae.
- Lichen planus is a self-limiting disease that goes away in months, though it can recur while LPP is long-lasting and can progress for years and decades.
It is diagnosed by examination, examination under the microscope, and skin biopsy. Topical steroids, antihistamines, antibiotics, and immunosuppressive drugs are helpful in treatment.
Important Red Flags of Large Plaque Parapsoriasis
Although large plaque parapsoriasis is usually harmless and remains dormant for many years, but in some cases, it can progress into mycosis fungoides or cutaneous T-cell lymphoma. So once LPP is diagnosed, it should be treated as early as possible to reduce the risk of its progression to life-threatening carcinoma.
