Contents
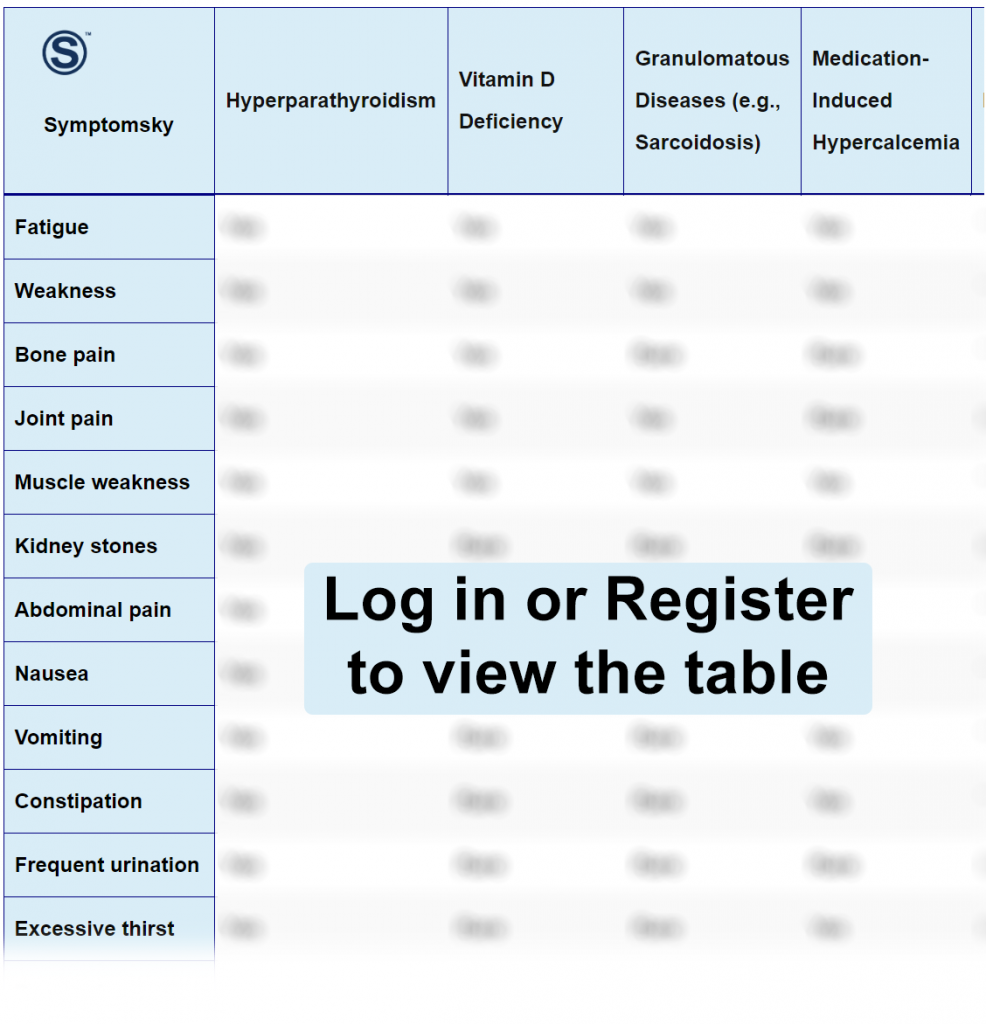
- 1 Hyperparathyroidism Differential Diagnosis Table:
- 2 How to Distinguish Hyperparathyroidism from Other Diseases
- 2.1 Distinguish Vitamin-D Deficiency from Hyperparathyroidism – Diagnosis
- 2.2 Distinguish Granulomatous Diseases from Hyperparathyroidism – Diagnosis
- 2.3 Distinguish Medication-Induced Hypercalcemia from Hyperparathyroidism – Diagnosis
- 2.4 Distinguish Malignancy from Hyperparathyroidism – Diagnosis
- 2.5 Distinguish Familial Hypocalciuric Hypercalcemia from Hyperparathyroidism – Diagnosis
- 2.6 Distinguish Primary Hyperaldosteronism from Hyperparathyroidism – Diagnosis
- 3 Hyperparathyroidism Complications and Treatment
Hyperparathyroidism Differential Diagnosis Table:
The parathyroid gland is four glands embedded in the posterior aspect of the thyroid gland. The parathyroid gland is responsible for calcium homeostasis. Hyperparathyroidism is an endocrine disorder resulting in excessive production of parathyroid hormone (PTH), leading to hypercalcemia.
Hyperparathyroidism causes nephrolithiasis (kidney stones), nephrocalcinosis (deposition of calcium salts in parenchyma and tubules of the kidney), along with other signs and symptoms such as muscle weakness, fractures, bone pain, hypertension, confusion, altered mental states, etc. Hyperparathyroidism is diagnosed through laboratory tests as serum calcium and PTH levels, and also through imaging (Tumor) as ultrasonography and Parathyroid-nuclear medicine scans.
Hyperthyroidism in the first stages is asymptomatic until serum calcium levels exceed 12 mg/dL and the patient starts to experience cardiac arrhythmias, dehydration, constipation, anorexia, polyuria, and polydipsia.
How to Distinguish Hyperparathyroidism from Other Diseases
Distinguish Vitamin-D Deficiency from Hyperparathyroidism – Diagnosis
- Kidney stones are absent in vitamin D deficiency, yet they are present in hyperparathyroidism.
- Vitamin-D deficiency is associated with decreased levels of calcium, while hyperparathyroidism is associated with increased levels of calcium.
“Vit-D serum levels are used for differentiation.”
Distinguish Granulomatous Diseases from Hyperparathyroidism – Diagnosis
- Granulomatous disease is associated with skin manifestations and recurrent pneumonia, unlike hyperparathyroidism, which is not associated with these signs.
- Granulomatous disease is non-caseating granuloma, while hyperparathyroidism does not cause granuloma.
“Laboratory tests such as CBC and liver function tests and Radiographic tests such as CT-chest and SPECT.”
Distinguish Medication-Induced Hypercalcemia from Hyperparathyroidism – Diagnosis
- Medication-induced hypercalcemia is not associated with kidney stones, while hyperparathyroidism is associated with kidney stones.
- Medication-induced hypercalcemia can be treated with medication cessation, unlike hyperparathyroidism, which is not connected to medication.
“Patient medication-history is used for differentiation.”
Distinguish Malignancy from Hyperparathyroidism – Diagnosis
- In Malignancy, hypercalcemia exceeds 13 mg/dL, while in hyperparathyroidism, mild hypercalcemia occurs.
- Malignancy is associated with the presence of cancerous tumor, while hyperparathyroidism is not associated with a cancerous tumor.
“Biopsy and tumor markers are used for differentiation.”
Distinguish Familial Hypocalciuric Hypercalcemia from Hyperparathyroidism – Diagnosis
- Familial hypocalciuric hypercalcemia is a genetic disorder with normal PTH, while hyperparathyroidism is an endocrine disorder with high levels of PTH.
- Familial hypocalciuric hypercalcemia is asymptomatic, while hyperparathyroidism is associated with many signs and symptoms.
“Urinary calcium/creatinine clearance ratio is used for differentiation.”
Distinguish Primary Hyperaldosteronism from Hyperparathyroidism – Diagnosis
- Primary hyperaldosteronism results in two complications: uncontrolled hypertension and hypokalemia, unlike hyperparathyroidism where hypertension rarely occurs and there is an absence of hypokalemia.
- Primary hyperaldosteronism is not accompanied with musculoskeletal manifestations, while musculoskeletal manifestation is a crucial sign and symptom in hyperparathyroidism.
- Primary hyperaldosteronism does not have renal, gastrointestinal, and neurological manifestations, while hyperparathyroidism is associated with renal (kidney stones), gastrointestinal (vomiting and constipation), and neurological (confusion and altered mood states).
“Morning elevated aldosterone to plasma renin test is used for differentiation.”
Hyperparathyroidism Complications and Treatment
Parathyroid crisis is a life-threatening sudden episode of hypercalcemia (in patients with hyperparathyroidism), where calcium levels dramatically increase to exceed 15 mg/dL, leading to a coma and death. This condition is treated as an emergency.
Surgery is a definitive treatment in primary hyperparathyroidism, yet some older patients with mild hypercalcemia and no complications are applicable to pharmacological treatment by bisphosphonates and/or cinacalcet, in addition to non-pharmacological treatment such as limiting calcium intake. In case of secondary hyperparathyroidism, where the patient is vitamin D deficient, the patient should receive a daily intake of 1,000 IU of vitamin D.
