What is causing my headache? How to find the cause for my headache?
What Type of Headache Do You Have? Migrane vs Tension and Cluster?
Contents
- 1 Headache Differential Diagnosis Algorithm
- 2 Headache Differential Diagnosis Table
- 3 How to Distinguish Migraine from Other Disease
- 3.1 Distinguish Tension-Type Headache from Migraine – Diagnosis
- 3.2 Distinguish Cluster Headache from Migraine – Diagnosis
- 3.3 Distinguish Hypertension from Migraine – Diagnosis
- 3.4 Distinguish Stroke from Migraine – Diagnosis
- 3.5 Distinguish Sinusitis from Migraine – Diagnosis
- 3.6 Distinguish Subarachnoid Hemorrhage from Migraine – Diagnosis
- 3.7 Distinguish Meningitis from Migraine – Diagnosis
- 3.8 Distinguish Medication-Overuse Headache from Migraine – Diagnosis
- 3.9 Distinguish Temporal Arteritis from Migraine – Diagnosis
- 3.10 Distinguish Cervicogenic Headache from Migraine – Diagnosis
- 3.11 Distinguish Trigeminal Neuralgia from Migraine – Diagnosis
- 3.12 Distinguish Acute Glaucoma from Migraine – Diagnosis
- 3.13 Distinguish Temporomandibular Joint Disorders from Migraine – Diagnosis
- 4 Important Red Flags in Migraines
- 5 Additional Information:Each Disease That Causes Headache Explained
- 6 Additional Headache Resources:
Headache Differential Diagnosis Algorithm
We’ll take a methodical approach to headache differential diagnosis; we’ll also attempt to explain various results and potential reasons for headaches, and we’ll also explain the warning signs from the source of headaches.
If a patient complains of a headache, the first question you ask is whether they can describe it as a thunderclap type of headache.
This is because a thunderclap headache is a strong headache that comes out of nowhere and reaches its peak severity in a matter of seconds or minutes. This kind of headache is linked potentially to harmful disorders, including cerebral venous sinus thrombosis and subarachnoid hemorrhage, which is a type of bleeding in the brain.
Therefore, it is crucial that headache patients undergo accurate diagnostics to detect glaucoma. Now we’ll get to know common forms and types of headaches that we have, such as migraine, tension headache, the most prevalent type of headache, and cluster headache, which is extreme pain that appears in clusters. We’ll be able to rule out some of these dangerous conditions through the process of differential diagnosis.
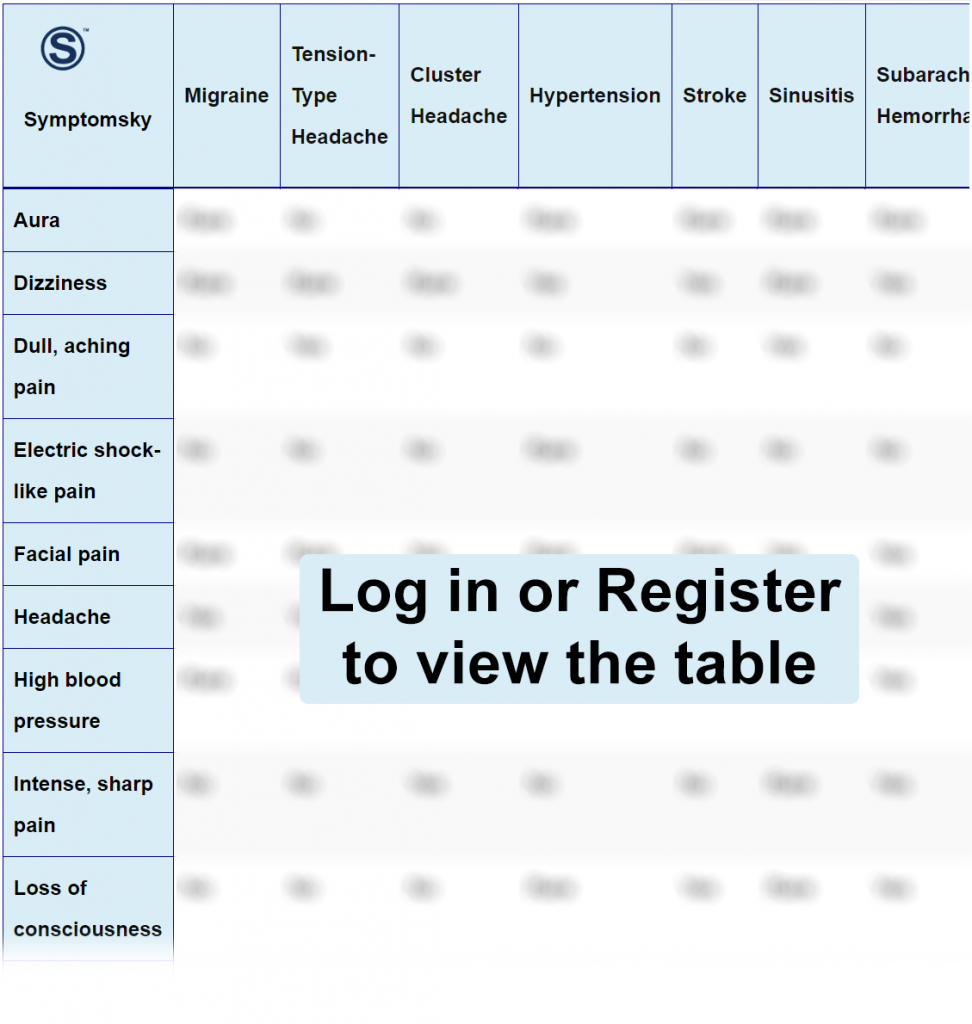
Headache Differential Diagnosis Table
Migraine is a complex neurological condition affecting millions of people worldwide. The term “migraine” came from the Greek word “hemikrania,” meaning half skull, owing to its characteristic unilateral headache.
Migraines usually present themselves as recurrent unilateral mild to severe headaches accompanied by nausea, visual disturbance, heightened sensitivity to light and sound. In some instances, it sends warning signs, known as aura, before actually appearing. This is called migraine with aura. Other common types include migraine without aura and chronic migraine.
How to Distinguish Migraine from Other Disease
Distinguish Tension-Type Headache from Migraine – Diagnosis
Tension-type headache is a type of headache that affects the forehead and temple and often feels like a band around the head.
- Both can be differentiated on the basis of the severity of pain. Usually, migraines cause more severe pain compared to tension-type headaches.
- Moreover, tension-type headaches are almost always bilateral, unlike migraines, which are mostly unilateral.
- A typical episode of migraine usually lasts between 5 hours to 2 days; however, tension headaches stay for minutes to a day.
Distinguish Cluster Headache from Migraine – Diagnosis
Cluster headache, also known as suicide headache, is characterized by extremely severe, sharp, and stabbing unilateral pain in, behind, and around the orbital region and in the temple. The pain is so severe that it is compared to childbirth pain in the literature.
- The average attack of cluster headache ranges from 45 to 90 minutes. Whereas, migraine pain ranges between 5 hours to 72 hours.
- Almost 90% of the cluster headache patients show lacrimation, which is not that common in migraines.
- A very striking difference between the two is restlessness. Cluster headache patients are more agitated and active during the episode, while migraine patients usually prefer to rest throughout the attack.
Distinguish Hypertension from Migraine – Diagnosis
Hypertension is a condition of elevated blood pressure inside the systemic arteries. Elevated blood pressure can cause secondary headaches. This can present similarity to migraine, and both conditions can be confused with each other.
- Headache due to hypertension is almost always present with high systemic blood pressure, and it goes away after the blood pressure gets to normal. However, with migraine, elevated blood pressure is a rare finding.
- Other than that, hypertension headaches are usually accompanied by hypertension symptoms. Some of these symptoms like palpitations, sweating, fatigue, and confusion are not common with migraines.
- The symptoms like nausea, vomiting, phonophobia, and photophobia are rare findings in hypertensive headaches.
Distinguish Stroke from Migraine – Diagnosis
Stroke is a neurological condition resulting from the blockage of a vessel supplying blood to the brain or by hemorrhage inside the brain, resulting in brain damage.
- Stroke presents with typical symptoms like slurred speech, dizziness, weakness in the body, and unconsciousness. These symptoms are rare in migraine.
- Also, the headaches from strokes are sudden, unexplained, and intense. While migraine headaches usually present with aura.
“CT scan is the diagnostic tool that confirms a stroke. Moreover, a stroke with paralysis shows typical signs including the inability to smile, drooping on one side of the face, weakness, and inability to move one side of the body.”
Distinguish Sinusitis from Migraine – Diagnosis
The inflammation in the mucosal membrane of the paranasal sinuses is called sinusitis.
- Runny nose and facial pain are common symptoms of sinusitis. However, it is extremely rare to find these two with migraine.
- Moreover, sinusitis usually lasts for weeks, and migraines last only for hours or days.
Distinguish Subarachnoid Hemorrhage from Migraine – Diagnosis
Subarachnoid hemorrhage refers to bleeding surrounding the brain between the arachnoid membrane and pia mater, typically resulting from a ruptured aneurysm. One of the manifestations of subarachnoid hemorrhage is a severe headache often referred to as a “thunderclap headache” as its onset is sudden, severe, and peaks to maximum intensity in an hour.
- The symptoms are very similar to migraine, but subarachnoid hemorrhage usually has other symptoms mimicking a neurological problem like loss of consciousness, seizures, and vomiting.
- Migraines have an episodic nature, which presents with aura, usually unilateral, which starts gradually and produces throbbing pain. However, with subarachnoid hemorrhage, the pain is not episodic and extremely severe in nature that people describe it as the worst pain they ever felt.
- Neck pain is a common symptom in both conditions, but with subarachnoid hemorrhage, typical nuchal stiffness can be seen which makes the neck flexion limited.
“Computed tomography or a CT scan is a diagnostic difference which clearly shows a brain bleed and differentiates the two. Physical examination for neurological assessment with Brudzinski sign is positive when subarachnoid hemorrhage is present.”
Distinguish Meningitis from Migraine – Diagnosis
Meningitis is a life-threatening condition caused by the inflammation of the meninges covering the brain.
- Meningitis can present with fever and flu-like symptoms; however, migraines never present with these.
- Meningitis, in severe cases, can cause vision loss and double vision (diplopia).
- Meningitis can cause seizures, which can never be found with migraines.
“History along with physical examination, typically the neurological assessment by Kernig and Brudzinski sign, is often diagnostic of meningitis.”
Distinguish Medication-Overuse Headache from Migraine – Diagnosis
Medication-overuse headache is a neurological condition that develops as a secondary headache following the excessive use of analgesic medication to treat primary headache conditions like migraine and tension headache.
- Medication-overuse headaches usually last 15 or more than 15 days a month, with a history of pre-existing headaches. Migraine stays on average for some hours to 2 days.
- Since it is a chronic condition, a constant dull pain always exists or most days of the month. However, migraine pain is episodic and subsides between the episodes.
“With this headache history is often diagnostic. The patient is often taking analgesics (NSAIDs, ASA, and Acetaminophen) for 15 days and over-the-counter pain medication or a combination of pain medication 10 days for over 3 months.”
Distinguish Temporal Arteritis from Migraine – Diagnosis
Temporal arteritis is an inflammation of temporal arteries, usually mediated by giant cells.
- Temporal arteritis can cause a unilateral headache just like migraine, but unlike migraine, the skin over the affected side is also tender.
- In severe cases, temporal arteritis can lead to ocular ischemia leading to blindness. Migraine only causes mild visual disturbance during the attack.
- Moreover, temporal arteritis causes jaw claudication which makes chewing and talking difficult, unlike migraine.
“Upon palpation, a delayed pulse can be felt with temporal arteritis, a rare finding in migraine. Ultimately, temporal artery biopsy diagnoses temporal arteritis.”
Distinguish Cervicogenic Headache from Migraine – Diagnosis
Cervicogenic headache is a referred pain that initiates from neck movements.
- Cervicogenic headache is almost always associated with the neck, so pain in the neck, shoulder, and back are common symptoms with cervicogenic headache, a rare finding with migraine.
- Symptoms common to migraine like nausea, vomiting, phonophobia, photophobia, and visual disturbances are rarely found along cervicogenic headache.
Distinguish Trigeminal Neuralgia from Migraine – Diagnosis
Trigeminal neuralgia is defined as a sudden, sharp, burning, electric shock-like pain which lasts for a short duration, along the branches of the trigeminal nerve.
- Trigeminal neuralgia pain is usually sharp & severe, starts suddenly, and subsides within seconds to two minutes. Migraine, on the other hand, starts gradually, throbbing, and lasts for a longer duration.
- Trigeminal neuralgia pain is not strictly present along the temple or eye area. It can be along the cheek area or the jaw area. Migraine pain is only present along the eye and the temple region.
- Typical migraine symptoms like nausea, vomiting, phonophobia, and photophobia are not present with trigeminal neuralgia.
Distinguish Acute Glaucoma from Migraine – Diagnosis
Acute glaucoma is an obstruction of the aqueous humor of the eye, resulting in increased ocular pressure, which can lead to pain in the eyes.
- Acute glaucoma is mostly associated with pain in the eye and causes redness. Migraine pain usually involves the eye and temple. Moreover, it never causes redness in the eyes.
- Acute glaucoma can cause a rainbow-like halo when looking at light, which is not present with migraines.
“Clinical examination shows a cloudy or hazy cornea with acute glaucoma. Migraines do not make the cornea hazy.”
Distinguish Temporomandibular Joint Disorders from Migraine – Diagnosis
Temporomandibular joint disorders refer to any condition affecting the temporomandibular joint (TMJ), which is a joint between the mandible and skull.
- The joint is present in the auricular region just in front of the ears, and pain is typically present in this region, which can radiate to the head, shoulders, and neck. Migraines do not cause pain in the auricular region.
- These disorders do not cause nausea, vomiting, photophobia, and phonophobia, like migraines.
- Unlike migraines, people with these disorders have trouble chewing, speaking, and yawning.
- TMJ disorders are usually coupled with sensitivity of teeth; such a thing is not present with migraine.
Important Red Flags in Migraines
Migraines can be confused with potentially life-threatening conditions like stroke, subarachnoid hemorrhage, and meningitis. All these conditions are neurological and cause neurological symptoms like seizures, vomiting, confusion, dizziness, and fever (in meningitis). In addition to this, temporal arteritis and acute glaucoma can lead to blindness if not treated on time. Acute glaucoma causes red eyes with lacrimation along with a headache. Similarly, temporal arteritis causes tender skin and jaw claudication.
These symptoms, when present with a headache, should be dealt with caution as they can lead to serious consequences.
Additional Information:
Each Disease That Causes Headache Explained
Tension Headache:
In this video we explained tension type of headache and how to recognize it. We also explaind its differences from other types of headache. It's important to understand that we have a video about headache algorithm video and you can watch it on our website.
Posted by Symptomsky – Medical Chat & USMLE-prep on Monday, September 18, 2023
Tension headaches are dull pain or pressure like bilateral tightness that can feel like squeezing of the skull. As the name suggests, they are also called stress headaches.
It usually affects females like migraine but the differentiating feature is it does not last longer than 4 to 6 hours.
Its intensity is bearable from light to moderate pain or pressure in the front, top, or sides of your head. Systemic effects associated with this type of headache like nausea and vomiting are also negligible.
Tension headaches typically manifest without prodrome or aura related warning signs.
Episodic tension headaches happen fewer than 15 days per month while chronic ones happen more than 15 days per month.
Coming to therapy options.
In acute tension headaches, we can use Acetaminophen, Aspirin and Ibuprofen to relieve pain.
For prevention of tension headaches we use tricyclic antidepressants containing Amitriptyline, doxepin and clomipramine and you can also try tricyclic antidepressants incase of failure.
Migrane:
In this video I explained how migrane can be recognized. Something that sets it apart from other types of migranes is it's throbbing pain that appears only unilaterally. The Migrane itself also lasts longer than the cluster type of headache and some common trigger factors have been identified. Something really frustrating with migrane is that one cannot easily identify the trigger factors since they sometimes trigger the attack and sometimes don't. I have a close relative who sufferes from migrane attacks and did notice a connection to lack of sleep or disturbed sleep patterns but also cheese and chocholate. Preventing migrane attacks usually includes a reduction of these trigger factors but also medications such as betablockers (metoprolol and bisoprolol). Acutely one can administer NSAIDs and metoclopramide and CGRP-antibodies (erenumab, fremanezumab). In the end it's important to remember that there is no definiteve diagnostic test for migrane but a symptom that truly helps us identify it are the prodorme and aura which appear prior to the migrane attack.
Posted by Symptomsky – Medical Chat & USMLE-prep on Tuesday, September 19, 2023
So we are going to talk about migraine and as you know migraine is just one type of headache and there are different types of headaches. And we are going to talk about migraine, how to recognize it and how to treat it. Migraine is type of headache that is characterized by pulsating, throbbing unilateral headache. Now patients with migraine usually exhibit photophobia and phonophobia. Now the literal meaning of these words mean fear of light or a fear of sound. the patients don’t experience fear of light or a fear of sound, but they rather overly sensitive to sound and light stimuli. So the patients who suffer from migraine attacks usually describe Prodrome and Aura and Prodrome basically stands for early signs changes that might be noticed before the patient experiences a migraine headache. So for example the patient might report that they suffer from constipation, mode changes but sometimes like mode swings from depression to euphoria. Patients sometimes also describe mix deafness. And when we are talking about Aura we are basically referring to vision changes that patient notice. they are mostly visual temporary disturbances but they can also be sensory disturbances as well. So normally in migraine attack can lasts from 4 hours to 3 days and it happens periodically. Now patients suffering from migraine attacks are more commonly female and also physical work can make a migraine attack worse and the migraine attack itself or migraine disease reduces physical and intellectual performance of the patients. Now when we look at cyesommon triggers that is what can trigger not cause but trigger migraine attack, in migraine attack we are looking at stress, cheese, chocolate, lack of sleep and alcohol, here we don’t have physical work because physical work itself in a healthy life style is not something that triggers migraine attacks. Now some extreme form of physical work might trigger migraine attack but normal healthy workout as well as diet is definitely recommended in patients with migraine. Now if we look at the therapy options for migraine, we have to distinguish between therapy options for acute migraine attacks and prevention of these migraine attacks. So if the patient already experiences acute migraine attack, we can use NSAIDs as well as antiemetics such as metoclopramide. Now NSAIDs they are standard first line pain killers and metoclopramide is used because with migraine often report vomiting and nausea. So far so good but what if that fails, well if the initial treatment fails. then we can use triptans (sumatriptans, zolmitriptan and dihydroergotamine). What if we want prevent acute migraine attacks in such case we have to address the triggers that are known to cause migraine attacks and those include stress, cheese, chocolate lack of sleep and alcohol. So obviously the patient should have regular sleep and avoid triggers such as stress , cheese, chocolate and alcohol. What about medications, well there are different medications that can be used to prevent migraine attacks but this should be decided case by case bases because these medications has side effects and it has to be decided each separate case whether they should be used or not. So the medications that they are commonly used as prevention from migraine attacks are (metoprolol and bisoprolol), topiramate and amitriptyline. Furthermore if the patient experiences more than 4 migraine attacks per month :CGRP-Antibodies (Erenumab Fremanezumab). Now migraine is only one type of headache and there are different types of headaches that we discussed in our algorithm videos. Hopefully this helping you identifying what is causing the headache and recognize emergency signs and red flags.
Cluster Headache:
Here I have attempted to explain the basics of cluster headache for the USMLE. Cluster headache presents with cluster attacks and that is something that is widely known. But what is often not known is that this headache can be confused with Hemicrania continua and SUNCTH syndrome. This is my first attempt to explain this topic and it's basically our prep for the USMLE step 1 exam. We tried to provide information as accurate as possible. In our algorithm for the cluster headache, we attempted to explain how it differs from migrane and tension headache as well. It is never too late to attempt to explain this properly. Sincerely yours Symptomsky
Posted by Symptomsky – Medical Chat & USMLE-prep on Wednesday, September 20, 2023
Cluster Headache is a type of headache that occurs in clusters which is extremely painful. It can be more severe than a migraine. Like a tension headache, it does not last longer but it is always unilateral and peri orbital.
We get a cluster headache when a cranial nerve pathway in the base of our brain is triggered.
The general signs and symptoms include, runny or congested nose, red warm face, sweating red and swollen or drooping eye associated with Horner syndrome and eyelid edema.
The hallmark is these clusters episodes tend to occur during nighttime hours. Within these cluster periods, patients may experience multiple attacks per day.
Differentiating it from other similar diagnoses like Hemicrania continua is characterized by low level of discomfort in the head. while SUNCT syndrome is different from cluster headache by its shorter attacks that happen more frequently.
Therapy for acute and chronic cases are different.
We give 100% oxygen, Sumatriptan and Lidocaine for acute relief while chronic therapy includes Verapamil, Lithium carbonate and Lidocaine (nasal).
