Contents
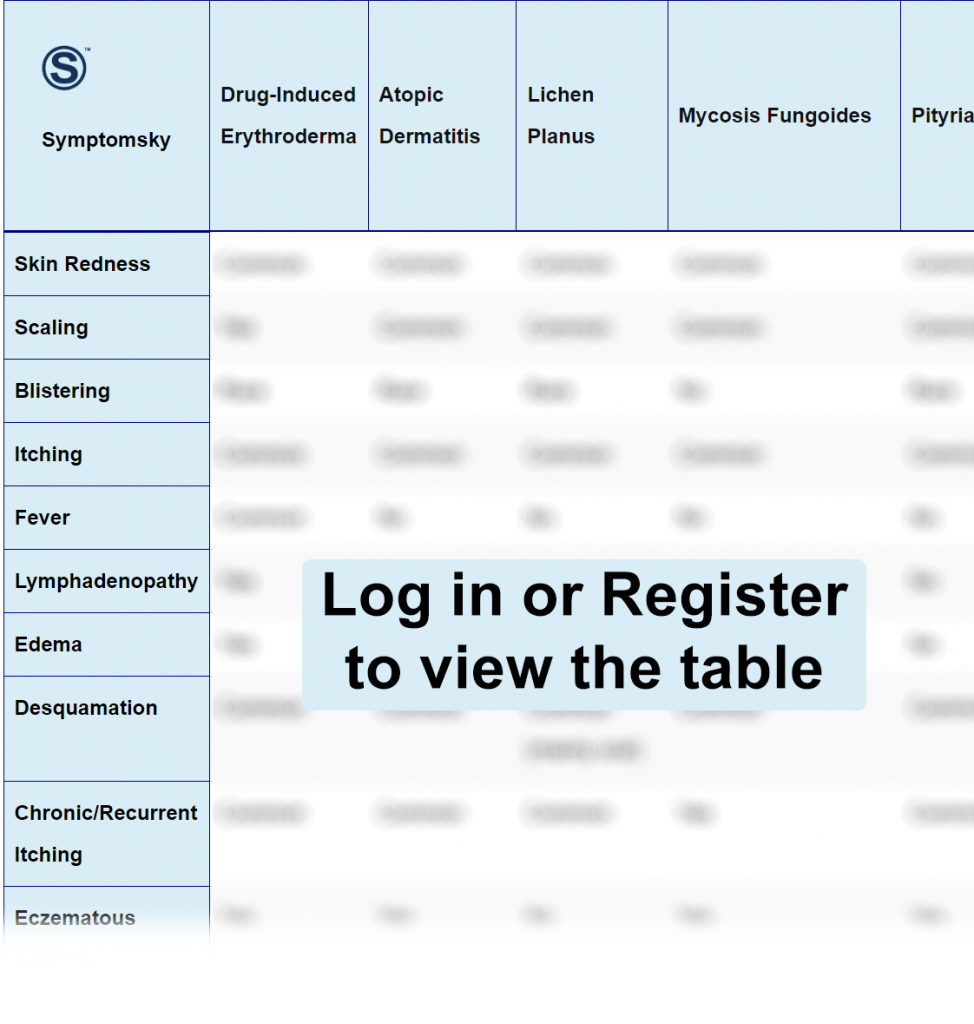
- 1 Drug-Induced Erythroderma Differential Diagnosis Table:
- 2 How to Distnguish Drug-Induced Erythroderma from Other Diseases
- 2.1 Distinguish Atopic Dermatitis from Drug-Induced Erythroderma – Diagnosis
- 2.2 Distinguish Lichen Planus from Drug-Induced Erythroderma – Diagnosis
- 2.3 Distinguish Mycosis Fungoides from Drug-Induced Erythroderma – Diagnosis
- 2.4 Distinguish Pityriasis Rubra Pilaris from Drug-Induced Erythroderma – Diagnosis
- 2.5 Distinguish Sézary Syndrome from Drug-Induced Erythroderma – Diagnosis
- 2.6 Distinguish Urticaria from Drug-Induced Erythroderma – Diagnosis
- 2.7 Distinguish Scarlet Fever from Drug-Induced Erythroderma – Diagnosis
- 2.8 Distinguish Staphylococcal Scalded Skin Syndrome from Drug-Induced Erythroderma – Diagnosis
- 2.9 Distinguish Acute Generalized Exanthematous Pustulosis (AGEP) from Drug-Induced Erythroderma – Diagnosis
- 2.10 Distinguish Acute Graft-versus-Host Disease (aGVHD) from Drug-Induced Erythroderma – Diagnosis
- 2.11 Distinguish Exanthematous Drug Eruption from Drug-Induced Erythroderma – Diagnosis
- 3 Important Red Flags in Drug-Induced Erythroderma
Drug-Induced Erythroderma Differential Diagnosis Table:
Erythroderma is an extensive wide inflammation and redness in the skin, in most of the body parts. The skin loses much fluid, salts, and proteins, making it a life-threatening condition that requires immediate medical intervention.
Erythroderma itself is not a disease but a symptom or a condition that results from a variety of diseases, including a reaction from a drug.
Drug-induced erythroderma can result from a wide range of drugs, including NSAIDs, ACE inhibitors, anti-epileptics, antifungal, antidepressants, etc.
The drug usually causes a severe reaction inside the body, resulting in vasodilation and starting a chain of stimulating inflammatory markers.
How to Distnguish Drug-Induced Erythroderma from Other Diseases
Distinguish Atopic Dermatitis from Drug-Induced Erythroderma – Diagnosis
Atopic dermatitis, also known as eczema, is a chronic skin condition that appears in childhood mostly and results from an allergic reaction when your skin comes in contact with something your body is allergic to. It causes itching and redness in the skin. The best treatment for atopic dermatitis is to prevent the disease and stay away from the allergen itself.
- The main difference between erythroderma and atopic dermatitis is that erythroderma is an extensive form of atopic dermatitis that covers the whole body, while atopic dermatitis covers only a small part where your skin comes in contact with the allergen.
- A skin biopsy may be needed if your doctor isn’t sure of the diagnosis, and a small piece of your skin will be taken and examined.
Distinguish Lichen Planus from Drug-Induced Erythroderma – Diagnosis
Lichen Planus is a skin inflammatory disease that affects several parts of the body. It has an idiopathic origin, and some people link it to the immune system. It often appears as clusters of red patches or papules, and some people link it to other diseases like the hepatitis C virus.
- A skin biopsy can easily diagnose lichen planus, and it’s the main diagnostic test.
Distinguish Mycosis Fungoides from Drug-Induced Erythroderma – Diagnosis
Mycosis Fungoides is a type of cutaneous T-cell lymphoma, one of the most common types of blood cancer that affects white and T-cells. Mycosis fungoides causes pink and raised scaly lesions on the skin, although these lesions are not actually cancerous.
Mycosis fungoides is mainly diagnosed and differentiated from other diseases by:
- T-cell receptor gene rearrangement: It’s a test in which T-cells in the blood are checked to see if there are any changes in genes that form the T-cell receptor.
- DNA flow cytometry: To determine any changes in DNA or the number of chromosomes.
- Biopsy: Either a skin biopsy or a biopsy from lymphatic tissue is taken to be examined.
“First, a physical examination and evaluation from doctors are made, and blood tests are usually needed.”
Distinguish Pityriasis Rubra Pilaris from Drug-Induced Erythroderma – Diagnosis
Pityriasis rubra pilaris (PRP) is a chronic rare skin condition, in which the skin becomes inflamed, red, and scaling may occur. It usually starts on the face then disseminates to the rest of the body. This condition can be classified into six types, and its cause is usually unknown. If PRP disseminates to cover most of the skin, it will look exactly like drug-induced erythroderma. Some doctors say that PRP is not easily diagnosed.
- Since the diagnosis by physical examination is often hard, a biopsy is usually needed to confirm the diagnosis.
“PRP is often accompanied by changes in nails, where your doctor will likely examine first if they suspect PRP. Another thing in PRP, there’s a signature unaffected skin, which is named island of sparing, which is unique to this disease.”
Distinguish Sézary Syndrome from Drug-Induced Erythroderma – Diagnosis
Just like mycosis fungoides, Sezary syndrome is also a type of cutaneous T-cell lymphoma. It’s a very aggressive form of blood cancer, and its skin lesions are not cancerous as well. Alopecia and edema are common symptoms of the disease as well.
- Peripheral blood smear: showing Sezary cells is the most diagnostic test for Sezary syndrome. Sezary cells have a unique morphology that can be detected by pathology labs and confirm the diagnosis.
- A biopsy: may be needed to confirm the diagnosis in some cases.
- T-cell receptor gene rearrangement: It’s a test in which T-cells in the blood are checked to see if there’s any change in genes that form T-cells receptor.
- DNA flow cytometry: to determine any change in DNA or number of chromosomes.
“Sezary syndrome and mycosis fungoides are often mistaken for each other as they both are subtypes of cutaneous T-cell lymphoma, but Sezary syndrome has its characteristic Sezary cells while mycosis fungoides don’t.”
Distinguish Urticaria from Drug-Induced Erythroderma – Diagnosis
Urticaria, often known as hives, is an allergic skin reaction that usually causes redness, itching, and skin welts. It is also often accompanied by angioedema, and some link it to autoimmune diseases as well. Hives can be both acute, which will fade away on its own within 24 hours, or chronic.
- Your doctor will likely diagnose hives by clinical examination and medical history. The hard part is knowing what causes the hives.
- Skin prick test, where your doctor will contact your skin with different types of allergens, may also be used.
- Blood test to confirm the presence of antibodies in your blood.
Distinguish Scarlet Fever from Drug-Induced Erythroderma – Diagnosis
Scarlet fever is a rash caused on the skin by a strep throat infection. It usually affects children from ages 5 to 15 years old and causes symptoms that look like the flu with a fever and red raised bumps on the skin that affect most of the body. Scarlet fever can be treated with antibiotics easily.
- Throat swab culture for the detection of streptococcal infection can easily diagnose scarlet fever, and it’s the gold standard diagnostic test for scarlet fever.
- Rapid Antigen Detection Test (RADT) has high specificity with low sensitivity toward streptococcal infection.
“Scarlet fever causes swelling in neck glands and red bumps on the tongue called strawberry tongues, which helps the doctor make a diagnosis.”
Distinguish Staphylococcal Scalded Skin Syndrome from Drug-Induced Erythroderma – Diagnosis
Staphylococcal Scalded Skin Syndrome (SSSS) is a serious skin infection caused by the toxins of staphylococcal organisms. It causes the skin to peel and form blisters, sometimes progressing very hard and causing hemodynamic instability. The disease most commonly affects infants, but sometimes it can affect older individuals, especially those who are immunocompromised or people with severe renal disease.
- Cultures from the pharynx, urine, and blood may be taken to confirm the diagnosis by detecting Staphylococcus organisms.
- Sometimes a skin biopsy may be needed for final confirmation.
“Nikolsky sign, which is a skin test where the top layer of the skin is removed when rubbed, is positive in SSSS, but it’s also positive in other skin conditions. Still, it can help limit the differential diagnosis.”
Distinguish Acute Generalized Exanthematous Pustulosis (AGEP) from Drug-Induced Erythroderma – Diagnosis
Acute Generalized Exanthematous Pustulosis is a severe skin adverse reaction caused by medication, especially antibiotics, but sometimes it can be caused by viral infections like EBV. It’s a type 4 hypersensitivity reaction. AGEP forms superficial pustules on the skin.
- Blood tests to detect increased neutrophils and eosinophils can be used to help in the diagnosis.
- Patch tests by exposing the skin to the suspected causative organism are used.
- Rarely, a skin biopsy is needed to confirm the diagnosis.
- A drug re-challenge test can be used, but only when the benefits of diagnosis outweigh the risk of adverse reactions to the drug. It may be helpful to confirm the suspected causative agent.
“AGEP is a severe cutaneous adverse reaction to a drug; it’s classified as SCAR, which sometimes can be life-threatening.”
Distinguish Acute Graft-versus-Host Disease (aGVHD) from Drug-Induced Erythroderma – Diagnosis
Graft-versus-host disease develops after you receive stem cells from a donor. Your body may recognize the stem cells as a foreign body and attack them, causing a series of inflammatory reactions. GVHD has stages from (0 to IV), and the most common symptoms of acute GVHD are skin redness and itching. Sometimes, systemic symptoms such as nausea, vomiting, and diarrhea may occur.
- Diagnosis of aGVHD is based mainly on the presence of symptoms post-transplant.
- Tissue biopsy to detect any changes in organs is the confirmatory test that most institutions depend on.
- Liver function tests and pulmonary tests help in the evaluation of the disease.
Distinguish Exanthematous Drug Eruption from Drug-Induced Erythroderma – Diagnosis
Exanthematous drug eruption, also known as morbilliform drug eruption, is a severe allergic reaction to a drug, usually an antibiotic, that starts a few days after initiation of the drug. It causes red papules on the skin, and in severe cases, it may lead to erythroderma and low-grade fever.
- The diagnosis is mainly based on the clinical picture and past drug and medical history of the patient, excluding other possible causes like viral infection.
- Biopsy is not routinely done and, in most cases, not needed, but if there are many differentials, it may be required.
“Exanthematous drug eruption is much like viral exanthem, but the main difference between the two is the involvement of the mucosa in viral exanthem, and it most commonly occurs in children.”
Important Red Flags in Drug-Induced Erythroderma
Most of the time, erythroderma caused by drugs develops gradually over a few days. It begins as red patches until it covers the whole body. It’s important if you notice such a reaction after taking a drug for the first time to seek immediate medical attention. Erythroderma progresses very badly with systematic manifestation and hemodynamic stability. It has a high mortality rate. So, it’s important to see your doctor once you experience any of the previously mentioned symptoms.
