Contents
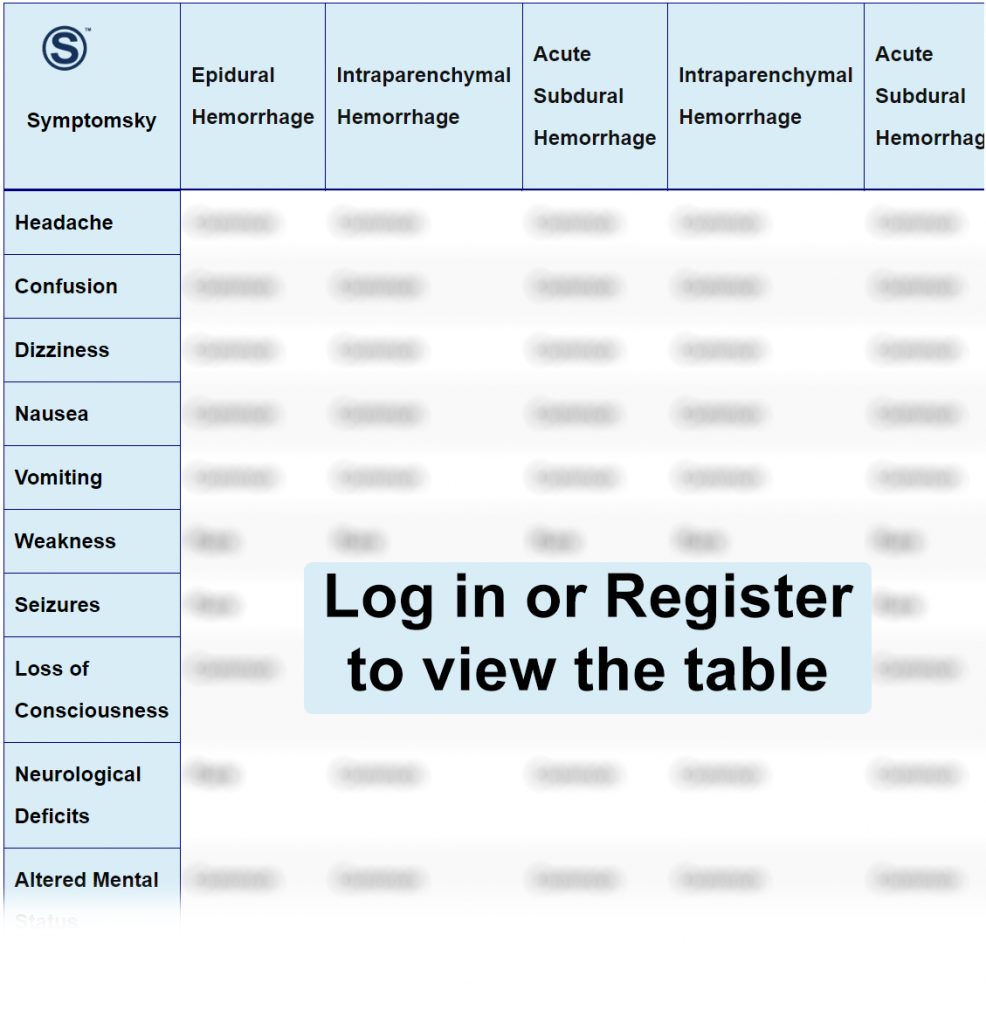
- 1 Epidural Hemorrhage Differential Diagnosis Table:
- 2 How to Distinguish Epidural Hemorrhage from Other Diseases
- 2.1 Distinguish Intraparenchymal Hemorrhage from Epidural Hemorrhage – Diagnosis
- 2.2 Distinguish Acute Subdural Hemorrhage from Epidural Hemorrhage – Diagnosis
- 2.3 Distinguish Subarachnoid Hemorrhage from Epidural Hemorrhage – Diagnosis
- 2.4 Distinguish Traumatic Brain Injury from Epidural Hemorrhage – Diagnosis
- 2.5 Distinguish Transient Ischemic Attack (TIA) from Epidural Hemorrhage – Diagnosis
- 2.6 Distinguish Seizures from Epidural Hemorrhage – Diagnosis
- 2.7 Distinguish Intracranial Abscess from Epidural Hemorrhage – Diagnosis
- 2.8 Distinguish Brain Tumor from Epidural Hemorrhage – Diagnosis
- 2.9 Distinguish Meningioma from Epidural Hemorrhage – Diagnosis
- 3 Important Red Flags in Epidural Hemorrhage
Epidural Hemorrhage Differential Diagnosis Table:
Epidural hemorrhage or epidural hematoma happens when a blood collection forms in the space between the skull and the outermost layer of the brain, which is called the “dura mater.”
It’s a life-threatening condition that requires rapid surgical intervention and evacuation of the blood collection.
Usually, epidural hemorrhage occurs as a result of a skull fracture that may cause an injury to a blood vessel, leading to vomiting, headache, and loss of consciousness.
MRI is the main diagnostic tool for diagnosing epidural hemorrhage and differentiating it from other types of hemorrhages or hematomas.
How to Distinguish Epidural Hemorrhage from Other Diseases
Distinguish Intraparenchymal Hemorrhage from Epidural Hemorrhage – Diagnosis
Intraparenchymal hemorrhage occurs when blood collects inside the dura itself. The most common cause of this type of hemorrhage is hypertension. We can differentiate intraparenchymal hemorrhage and epidural hemorrhage by:
- CT scan is the main diagnostic tool in all types of intracerebral hemorrhage.
- MRI.
Distinguish Acute Subdural Hemorrhage from Epidural Hemorrhage – Diagnosis
Subdural hemorrhage occurs rapidly within a few minutes after traumatic brain injury; your doctor will usually make the diagnosis based on:
- CT scan
- Assess the level of consciousness through the Glasgow Coma Scale (GCS), which will be severely decreased in this type of hemorrhage.
Distinguish Subarachnoid Hemorrhage from Epidural Hemorrhage – Diagnosis
Subarachnoid hemorrhage occurs when a brain aneurysm ruptures inside the blood vessels inside the brain. It’s a medical emergency, and if left untreated, may lead to permanent brain damage. Its most common symptom is a severe headache.
You can differentiate between epidural hemorrhage and subarachnoid hemorrhage by:
- CT scan
- Through lumbar puncture to analyze cerebrospinal fluid (CSF), by its appearance, it will look yellowish in color.
Distinguish Traumatic Brain Injury from Epidural Hemorrhage – Diagnosis
Traumatic brain injury occurs when an assault or damage occurs to the brain. It’s usually categorized as either closed TBI or penetrating TBI. The symptoms may appear immediately or may take several days to appear.
- Neurological examination is used primarily for the diagnosis of traumatic brain injury; the doctor will examine your motor and sensory function.
“MRI and CT scan cannot always detect traumatic brain injury, unlike other types of hemorrhage and hematomas.”
Distinguish Transient Ischemic Attack (TIA) from Epidural Hemorrhage – Diagnosis
Transient ischemic attack happens when the blood supply that delivers blood to the brain gets cut off. TIA usually resolves in less than one hour. Most of the time, TIA doesn’t cause permanent damage, and it has an underlying cause like hyperglycemia and hypertension.
- Neurological examination can be used to detect TIA.
- Carotid ultrasound may be used too if the doctor suspects that the cause of your TIA is blockage of the carotid artery.
- MRI is often used to detect TIA, unlike CT scans.
Distinguish Seizures from Epidural Hemorrhage – Diagnosis
Seizures are caused due to increased electrical activity in the brain. There are so many types of seizures; they usually affect your movement, and some can cause a decrease in consciousness. There are many causes of seizures, including brain infection like meningitis or maybe tumors or head injury. Seizures also differ in duration; they can last from seconds up to several minutes.
You can differentiate seizures from epidural hemorrhage:
- Electroencephalogram (EEG) is the most diagnostic test to confirm seizures from any other illness.
- MRI and CT scan can also be used to detect any focal points that are responsible for seizures.
“Seizures can be detected easily by physical appearance, but detecting the underlying cause may be challenging for finding the right treatment.”
Distinguish Intracranial Abscess from Epidural Hemorrhage – Diagnosis
Intracranial abscess is a pus collection inside the brain caused by an infection, either bacterial or viral, and in some rare cases, maybe a fungal infection. Surgical intervention and draining of the abscess may be required in some cases before starting antimicrobial therapy.
You can differentiate Epidural hemorrhage from intracranial abscess by:
- MRI and CT are usually used to detect intracranial abscess. If the diagnosis is made, CT-guided aspiration is usually performed to confirm the kind of infection and the organism causing the abscess.
- Blood culture is also performed to exclude the presence of sepsis or bacteremia.
- Lumbar puncture is used in most CNS infections for analysis of CSF.
Distinguish Brain Tumor from Epidural Hemorrhage – Diagnosis
Brain tumors are abnormal overgrowth of brain cells. This can either be benign or malignant tumors. Brain tumors are categorized into primary tumors, where they originate from the brain itself, or secondary tumors, where they metastasized from other body organs until they reach the brain.
Brain tumors can be diagnosed by:
- MRI and CT scan of the head are primarily used to diagnose the presence of any abnormalities in the brain.
- PET scan can be used to detect the presence of any cancerous tissue by the uptake of cells by radioactive iodine.
- Brain biopsy often requires surgery to be performed and has the risk of many complications and brain damage.
Distinguish Meningioma from Epidural Hemorrhage – Diagnosis
Meningioma is a slow-growing tumor that originates from the meninges, which is the outermost layer that surrounds the brain and spinal cord. It’s the most common tumor of the brain and usually takes years to be symptomatic and diagnosed.
- MRI or CT scan with dye is usually used to diagnose and confirm meningioma.
- Lumbar puncture can be used, which will usually show a high level of protein in CSF.
“The most common symptom of meningioma is a headache; in some cases, seizures and double vision can occur, which will require immediate medical attention.”
Important Red Flags in Epidural Hemorrhage
Epidural hematoma in most cases only happens due to trauma or injury to the head, so it’s important that after a brain injury, you seek medical attention. Your physician will likely order an immediate head CT to confirm or rule out Epidural Hemorrhage. You don’t need to worry since most epidural hemorrhages have a good prognosis, especially if evacuated early and are small in size.
