Contents
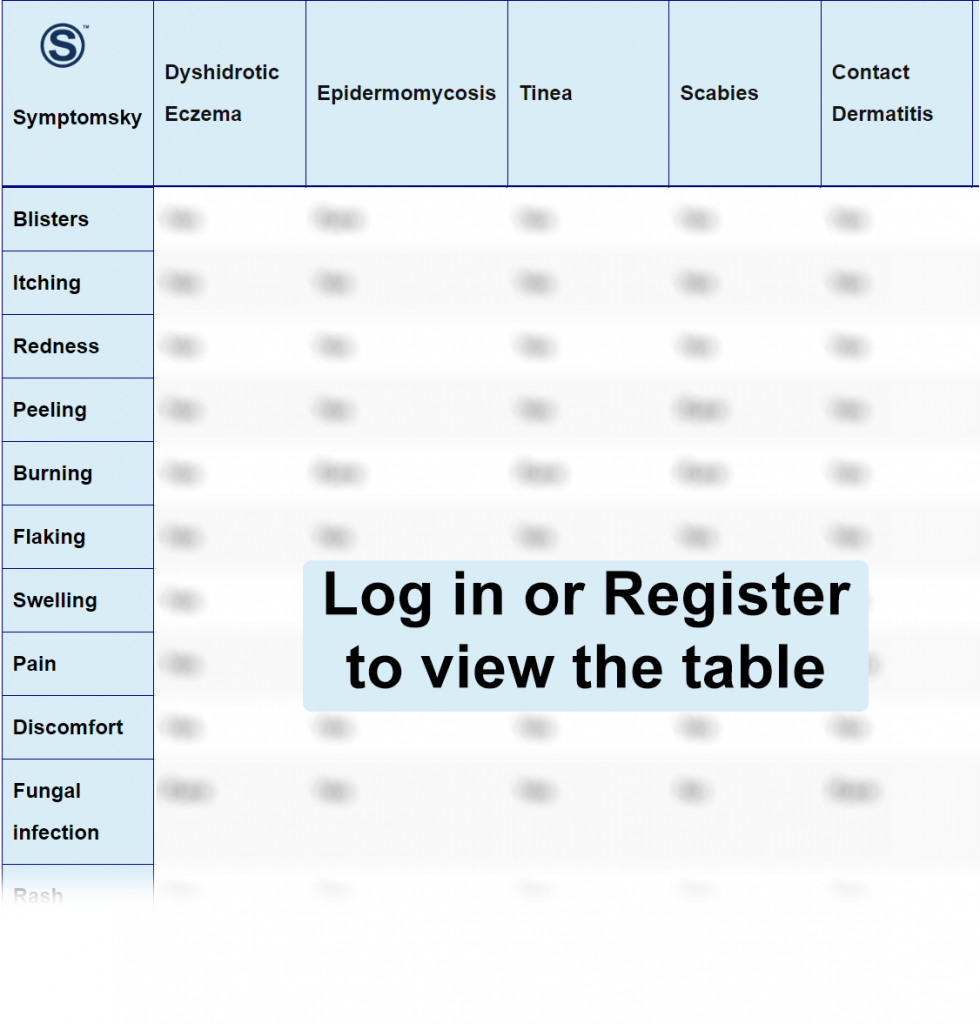
- 1 Dyshidrotic Eczema Differential Diagnosis Table:
- 2 How To Distinguish Between Dyshidrotic Eczema from Other Diseases
- 2.1 Distinguish Epidermomycosis from Dyshidrotic Eczema – Diagnosis
- 2.2 Distinguish Tinea from Dyshidrotic Eczema – Diagnosis
- 2.3 Distinguish Scabies from Dyshidrotic Eczema – Diagnosis
- 2.4 Distinguish Contact Dermatitis from Dyshidrotic Eczema – Diagnosis
- 2.5 Distinguish Bullous Pemphigoid from Dyshidrotic Eczema – Diagnosis
- 2.6 Distinguish Palmoplantar Pustular Psoriasis from Dyshidrotic Eczema – Diagnosis
- 3 Important Red Flags in Dyshidrotic Eczema
Dyshidrotic Eczema Differential Diagnosis Table:
Dyshidrotic eczema, or pompholyx, is a type of chronic skin eczema. Symptoms of dyshidrotic eczema include small, dry, itchy, and scaly patches of skin with blisters on the palms, soles, and sides of fingers. These blisters can cause severe itching, redness, and cracked skin, as well as crusting of blisters.
The cause of dyshidrotic eczema is idiopathic, but it is found to be associated with certain factors like irritants and an allergic reaction to metals, fungal infections, photosensitivity to light, smoking, and the use of OCPs. It is thought to be caused in people who lack a protein, Filaggrin, which is responsible for building a strong and protective skin barrier.
It is diagnosed based on the history and examination of the blisters. Patch tests, blood tests, or biopsies can also be performed. There is no definite cure for this disease, but corticosteroid creams and moisturization can help in relieving the symptoms.
How To Distinguish Between Dyshidrotic Eczema from Other Diseases
Distinguish Epidermomycosis from Dyshidrotic Eczema – Diagnosis
Epidermomycosis is a rare infection of the epidermis layer (stratum corneum) of the skin caused by dermatophytes. Causative agents for this disease are yeast and molds. The features that distinguish them from dyshidrotic eczema are:
- Epidermomycosis is caused by fungal infection, while dyshidrotic eczema is caused by an irritant or an allergen.
- Epidermomycosis is presented as a ring-shaped papule, which is inflamed and spreads peripherally, while dyshidrotic eczema presents as symmetrical, tiny vesicles that vary in size and shape.
- Epidermomycosis papules are mostly painless, while dyshidrotic eczema is quite painful and itchy.
Epidermomycosis is diagnosed based on history, clinical examination, blood tests, and culture can also be performed. It is treated with antifungal medication.
Distinguish Tinea from Dyshidrotic Eczema – Diagnosis
Tinea or Ringworm is a communicable disease caused by a fungal infection. It is found in warm and moist parts of the body such as the scalp, groin, underarms, beneath the breast, and feet. Symptoms of tinea are; ring-shaped, itchy rash having red, scaly, and cracked skin. The features that distinguish tinea from eczema are;
- Tinea is a fungal infection while dyshidrotic eczema is caused by an irritant or an allergen.
- Tinea is a contagious disease while dyshidrotic eczema doesn’t spread from person to person contact.
- Tinea or ringworm, as the name shows, has a ring-shaped rash with defined edges while dyshidrotic eczema rarely has a ring-shaped rash and can vary in size.
- Tinea affects areas with sweat like the groin and axillary part while dyshidrotic eczema spares these parts.
Tinea is diagnosed based on history and clinical examination. Skin scrapping can also be done. Tinea is treated with antifungal creams and lotions.
Distinguish Scabies from Dyshidrotic Eczema – Diagnosis
Scabies is a communicable disease caused by a severe itch-causing mite called Sarcoptes Scabies. Symptoms are intense itching and a severe itchy rash. The features that differentiate scabies from dyshidrotic eczema are;
- Sometimes, scabies and dyshidrotic eczema are hard to differentiate because of their similar rash, but the former is a contagious disease while the latter is a non-contagious disease.
- Scabies is caused by a mite that forms burrows in the skin while dyshidrotic eczema is caused by an irritant and an allergen.
- In scabies, itching flares up mostly at night while dyshidrotic eczema can flare up anytime.
- The rash of scabies is mostly present on finger webs and private parts while dyshidrotic rash is present on palms, soles, and sides of fingers.
Scabies is diagnosed based on history, clinical examination, and visualization of skin scrapping under a microscope. Permethrin 5% and 0.5 malathion lotion are used for the treatment of scabies.
Distinguish Contact Dermatitis from Dyshidrotic Eczema – Diagnosis
Contact Dermatitis, as the name suggests, is caused by contact with an irritant, a specific substance, or an allergic reaction to it. Symptoms are itchy rashes, hyperpigmented patches, bumps, and blisters that cause dry, flaky, and cracked skin. The features that distinguish contact dermatitis from dyshidrotic eczema are;
- Contact Dermatitis rash appears where the skin comes in contact with a specific irritant or substance while Dyshidrotic eczema can occur bilaterally.
- Contact Dermatitis has clear and specified borders while Dyshidrotic eczema rash can vary in size and shape.
- Contact dermatitis can be both acute and chronic, but it is mostly acute while Dyshidrotic eczema is a chronic condition.
Contact Dermatitis is diagnosed based on history and clinical examination while a patch test or clinical examination can also be performed. Contact dermatitis is treated with steroid creams and ointments.
Distinguish Bullous Pemphigoid from Dyshidrotic Eczema – Diagnosis
Bullous Pemphigoid is a rare, autoimmune condition of the skin. It causes large, itchy, hive-like welts and tense fluid-filled subepidermal blisters. These blisters, when ruptured, form crusted erosions. The features that distinguish them from dyshidrotic eczema are;
- Bullous Pemphigoid affects extremities at onset then moves to the trunk and flexures of the skin while dyshidrotic eczema mostly appears on palms, soles, and sides of fingers.
- Bullous Pemphigoid is an autoimmune disease while Dyshidrotic eczema is caused by certain irritants or an allergen.
- Bullous Pemphigoid affects older people, between 60 years to 80 years of age while dyshidrotic eczema can affect at any age but usually presents below 40 years of age.
Bullous pemphigoid is diagnosed based on history and examination but direct immunofluorescence (DIF) microscopy of a skin biopsy remains the gold standard. Antibiotics, corticosteroid creams, and lotions can be used for treatment.
Distinguish Palmoplantar Pustular Psoriasis from Dyshidrotic Eczema – Diagnosis
Palmoplantar Pustular Psoriasis (PPP), as the name suggests, is an uncommon, inflammatory, and chronic variant of pustular psoriasis that remains confined to palms and soles or both. The features that differentiate PPP from dyshidrotic eczema are;
- In PPP, vesicles contain pus while Dyshidrotic Eczema has fluid-filled vesicles.
- PPP and dyshidrotic eczema are both chronic conditions but the latter is a relapsing condition.
- PPP is an autoimmune disease and can affect the quality of life while Dyshidrotic eczema is not an immune-mediated disease.
History and physical examination can help in diagnosis but KOH preparations and biopsy can also be performed. Treatment can help in relieving the symptoms, but there is no definite cure for this disease.
Important Red Flags in Dyshidrotic Eczema
Dyshidrotic eczema is a relapsing condition but goes away without complication. Sometimes, in severe cases, it is superimposed by bacterial infection, which results in large blisters that spread to the back of hands and feet, which is quite painful, filled with pus, and can delay the healing process. It needs urgent treatment with antibiotics.
