Contents
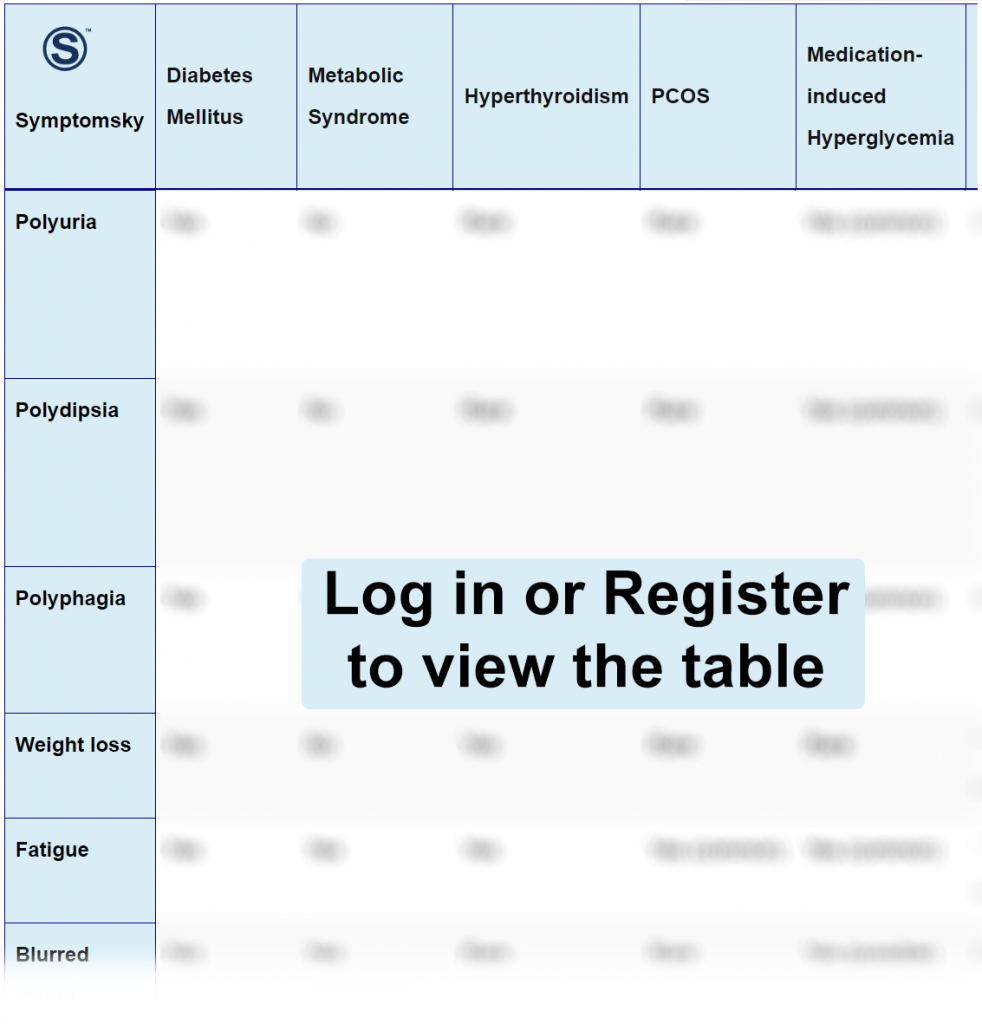
- 1 Diabetes Mellitus Differential Diagnosis Table:
- 2 How to Distinguish Diabetes Mellitus from other Diseases
- 2.1 Distinguish Metabolic Syndrome from Diabetes Mellitus – Diagnosis
- 2.2 Distinguish Hyperthyroidism from Diabetes Mellitus – Diagnosis
- 2.3 Distinguish PCOS from Diabetes Mellitus – Diagnosis
- 2.4 Distinguish Medication-Induced Hyperglycemia from Diabetes Mellitus – Diagnosis
- 2.5 Distinguish Pancreatitis from Diabetes Mellitus – Diagnosis
- 2.6 Distinguish Cushing Syndrome from Diabetes Mellitus -Diagnosis
- 2.7 Distinguish Hemochromatosis from Diabetes Mellitus -Diagnosis
- 2.8 Distinguish Diabetes Insipidus from Diabetes Mellitus – Diagnosis
- 2.9 Distinguish Diabetes Mellitus from Gestational Diabetes-Diagnosis
- 3 Diabetes Mellitus Red Flags and Management
Diabetes Mellitus Differential Diagnosis Table:
Diabetes Mellitus is a metabolic disease presented as elevated blood glucose levels. Diabetes mellitus has two types. Type-1, which is the destruction of beta-cells in the islets of Langerhans, which results in insulin absence. Type-2, which is an imbalance between insulin levels and insulin sensitivity.
The patient is diagnosed with DM after a history of elevated blood serum glucose random exceeding 200mg/dL, fasting exceeding 126mg/dL, and glycated hemoglobin equal to or more than 6.5%. Polyuria, polydipsia, and polyphagia are the main symptoms of DM, in addition to fatigue, blurred vision, skin dehydration, frequent yeast infection, and slow wound healing.
Diabetic patients should be educated about their disease to prevent complications and improve outcomes.
How to Distinguish Diabetes Mellitus from other Diseases
Distinguish Metabolic Syndrome from Diabetes Mellitus – Diagnosis
Metabolic Syndrome is the accumulation of multiple conditions due to the dysfunction of adipose tissue.
- Metabolic syndrome does not involve the main symptoms of diabetes, which are polyuria and polydipsia.
- Metabolic syndrome includes reduced HDL and elevated triglycerides, blood pressure, and glucose level, while Diabetes mellitus only includes elevated glucose level.
- Metabolic syndrome has a distinctive central weight gain, while diabetes is associated with overall obesity.
“Laboratory analysis such as serum triglycerides and HDL, in addition to history and physical examination, are used for differentiation.”
Distinguish Hyperthyroidism from Diabetes Mellitus – Diagnosis
Hyperthyroidism is a disease of excessive production of TSH.
- Hyperthyroidism is associated with hypertension, palpitations, tremors, dyspnea, and heat intolerance, which are all absent in diabetes mellitus.
“Laboratory analysis of TSH, total T3, and Free T4 are used for differentiation.”
Distinguish PCOS from Diabetes Mellitus – Diagnosis
Polycystic ovarian syndrome is an elevation in androgen levels in females.
- PCOS involves irregular menstruation as the main symptom; unlike diabetes mellitus, irregular menstruation cannot be present.
- PCOS includes acne, alopecia, hirsutism, and extreme pelvic pain, while diabetes mellitus does not include all of these symptoms.
“Pelvic ultrasound of ovarian cysts and blood analysis of hormones (FSH, LH, and GnRH).”
Distinguish Medication-Induced Hyperglycemia from Diabetes Mellitus – Diagnosis
Medication-induced Hyperglycemia is an alteration in insulin sensitivity and secretion.
- Medication-induced hyperglycemia is associated with drug administration (As hypertensive drugs), while diabetes hyperglycemia is not associated with drug administration.
“Glycated Hemoglobin blood analysis is used for differentiation.”
Distinguish Pancreatitis from Diabetes Mellitus – Diagnosis
- Pancreatitis is associated with severe acute abdominal pain radiating to the back accompanied by nausea and vomiting, while diabetes mellitus is not associated with abdominal pain.
“Abdominal imaging and blood analysis (serum lipase and Blood urea nitrogen) are used for differentiation.”
Distinguish Cushing Syndrome from Diabetes Mellitus -Diagnosis
Cushing syndrome is prolonged exposure to high cortisol levels.
- Cushing syndrome patients have a distinctive appearance of buffalo torso, moon face, thin arms, and legs, unlike diabetes mellitus, which does not have a distinctive appearance.
“24-hour urine free cortisol and late-night salivary cortisol tests are used for differentiation.”
Distinguish Hemochromatosis from Diabetes Mellitus -Diagnosis
Hemochromatosis is a condition of excess iron deposition. Symptom manifestations according to the organ affected.
- Hemochromatosis symptoms are associated with joint pain, while diabetes mellitus is not associated with joint pain.
“Serum transferrin blood test is used for differentiation.”
Distinguish Diabetes Insipidus from Diabetes Mellitus – Diagnosis
Diabetes insipidus is a decreased secretion in antidiuretic hormone.
- Diabetes insipidus is associated with dilute, glucose-free urine and normal blood glucose levels, while diabetes mellitus is associated with glucose in urine and hyperglycemia.
- Diabetes insipidus is accompanied by hypotension and tachycardia, unlike diabetes mellitus, which is not accompanied by hypotension nor tachycardia.
- Diabetes insipidus has clear symptoms of dehydration, while diabetes mellitus does not have symptoms of dehydration.
“Water deprivation and desmopressin blood analysis tests are used for differentiation.”
Distinguish Diabetes Mellitus from Gestational Diabetes-Diagnosis
Gestational diabetes is a disease of glucose intolerance during pregnancy.
- Gestational diabetes only occurs during pregnancy, while diabetes mellitus is not associated with pregnancy.
“Oral glucose tolerance test at 24-28 weeks of pregnancy is used for differentiation.”
Diabetes Mellitus Red Flags and Management
Uncontrolled diabetes mellitus complications are diabetic retinopathy (if left untreated leads to blindness), nephropathy (if left untreated leads to dialysis), neuropathy (if left untreated leads to amputation). Aggressive management should be avoided to prevent hypoglycemia that can be fatal.
Diabetes mellitus requires multiple interventions for management. Non-pharmacological interventions were found to improve outcomes through carbohydrates and calories restrictions, exercising, and glucose monitoring (maintenance 90-130mg/dL and HbA1c less than 7%). Pharmacological interventions should be customized according to each patient. In case of insulin absence, insulin administration is considered. In case of targeting insulin sensitivity or increasing insulin secretion, medications such as biguanides (metformin), glucagon-like-peptide-1-agonist, sulfonylureas, etc. are considered.
