Contents
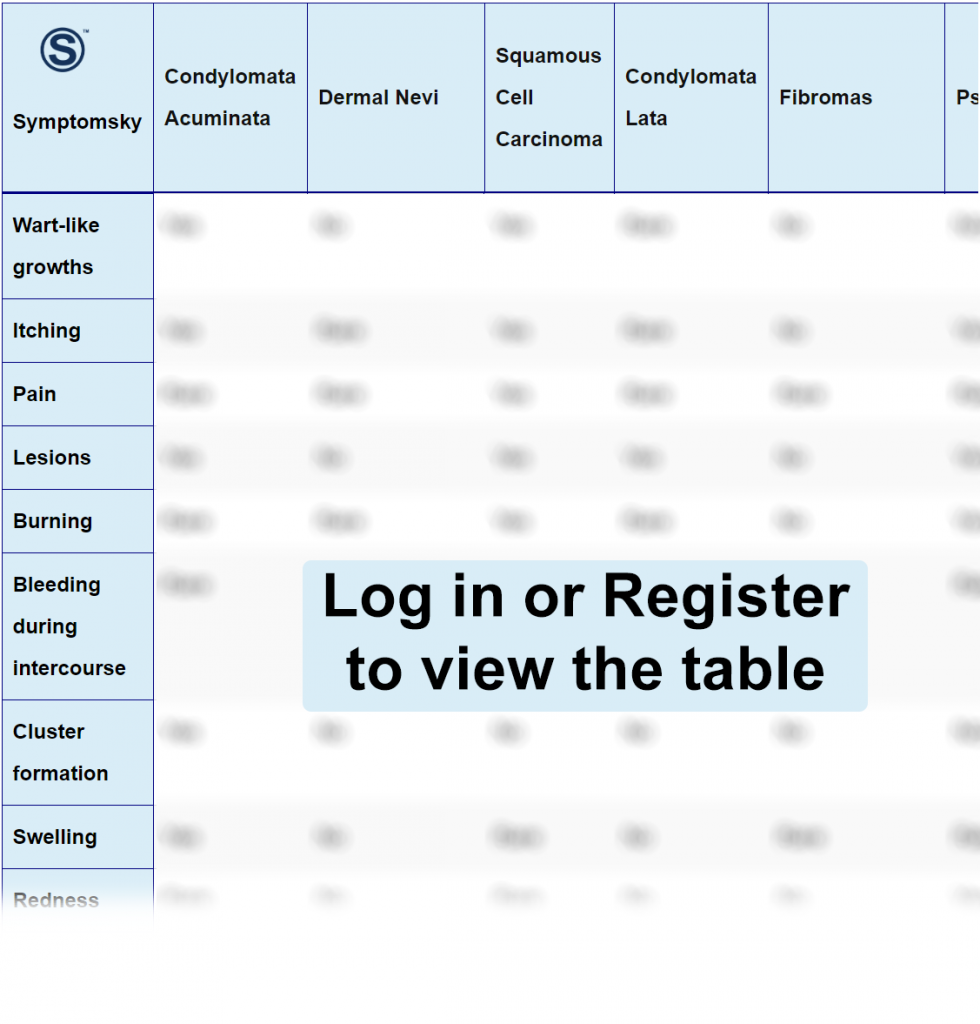
- 1 Condylomata Acuminata Differential Diagnosis Table:
- 2 How to Distinguish Condylomata Acuminata from Other Diseases
- 2.1 Distinguish Dermal Nevi from Condylomata Acuminata – Diagnosis
- 2.2 Distinguish Squamous Cell Carcinoma from Condylomata Acuminata – Diagnosis
- 2.3 Distinguish Condylomata Lata from Condylomata Acuminata – Diagnosis
- 2.4 Distinguish Fibromas from Condylomata Acuminata – Diagnosis
- 2.5 Distinguish Psoriasis from Condylomata Acuminata – Diagnosis
- 2.6 Distinguish Lichen Planus from Condylomata Acuminata – Diagnosis
- 2.7 Distinguish Molluscum Contagiosum from Condylomata Acuminata – Diagnosis
- 2.8 Distinguish Herpes Simplex Virus (HSV) from Condylomata Acuminata – Diagnosis
- 2.9 Distinguish Buschke-Lowenstein Tumor from Condylomata Acuminata – Diagnosis
- 3 Important Red Flags in Condylomata Acuminata
Condylomata Acuminata Differential Diagnosis Table:
Condylomata Acuminata is a viral infection that is most commonly known as genital warts. It’s caused by a low-risk virus called human papillomavirus (HPV).
It is transmitted mainly by sexual intercourse, and about 1% of sexually active people get infected by the virus, especially young populations between the ages of 20-30 years old.
Genital warts usually appear as white-pinkish papules on the genital area. They are often small in size, and in some cases, they disappear on their own.
Genital warts are often asymptomatic; they may cause some itching and, in rare cases, a burning sensation during peeing or bleeding during intercourse.
How to Distinguish Condylomata Acuminata from Other Diseases
Distinguish Dermal Nevi from Condylomata Acuminata – Diagnosis
Dermal Nevi are just harmless overgrowths of skin. They are just bumps in the skin with an overgrowth of melanin. They usually don’t require any medical attention unless their physical appearance bothers the patient, then they may ask a doctor for removal.
- Dermal nevi are usually diagnosed based on their appearance. You can differentiate them from Condylomata acuminata based on the characteristic cauliflower of genital warts.
- In some rare cases, a biopsy may be needed to confirm that the moles are benign growths of the skin.
Distinguish Squamous Cell Carcinoma from Condylomata Acuminata – Diagnosis
Squamous cell carcinoma is the second most common type of skin cancer. It’s an overgrowth of the skin that usually happens due to harmful exposure to UV lights and radiation that comes from the sun, lamps, or tanning.
When discovered early, squamous cell carcinoma of the skin can be easily managed and treated.
- Skin biopsy is the main diagnostic test for squamous cell carcinoma; your doctor will usually consider tissue biopsy after a physical examination.
- MRI and CT scan can help in diagnosis by identifying the size and growth of the cancer.
“Wearing sunscreen and avoiding tanning beds are important for the prevention of this kind of cancer.”
Distinguish Condylomata Lata from Condylomata Acuminata – Diagnosis
Condylomata Lata is a skin lesion that is associated with the sexually transmitted disease, syphilis. It’s the most known symptom of syphilis that usually appears in the early stage of the disease. And like genital warts, they appear on genital areas.
- Examination of the lesion under a dark-field microscope is usually used to confirm the disease by the characteristic appearance of condylomata lata.
- Biopsy can be used for differentiating Condylomata acuminata from condylomata lata.
- A blood test to detect syphilis antibodies can be used.
“Although both diseases are similar when it comes to genital warts, some differences can be seen: condylomata acuminata are usually dry warts while condylomata lata are wet. While condylomata acuminata has its characteristic cauliflower appearance, condylomata lata are usually smooth lesions.”
Distinguish Fibromas from Condylomata Acuminata – Diagnosis
Fibromas are noncancerous growths of connective tissues in the body. They are often harmless and don’t need any medical treatment. There are many types of fibromas: soft, hard, and angiofibroma, which are growths of connective tissue with blood vessels. Fibromas can develop in any part of the body: skin, organ, or bones.
- After a physical examination, your doctor will order an ultrasound to confirm the diagnosis of fibroma.
- MRI and CT scan can also be used for diagnosis, but the main diagnostic tool is ultrasound.
- In some rare cases, a biopsy may be needed to confirm the benign growth of fibroma.
- A major difference between fibromas and genital warts is that fibromas are bigger in size and fewer in number than genital warts.
“Uterine fibroids are a common type of fibroma that may cause symptoms in females, and medical treatment may be required for the improvement of symptoms, and in some cases, surgical intervention is needed.”
Distinguish Psoriasis from Condylomata Acuminata – Diagnosis
Psoriasis is an autoimmune chronic disorder that can’t be cured but can be managed and treated. The skin is renewed very fast, and it usually causes the characteristic silver scaly patches that can be easily diagnosed by doctors.
- Psoriasis’ main diagnostic test is the physical examination of the scales and patches on the skin. Since it’s very unique and characteristic to the disease itself, it makes it very easy to be diagnosed.
- In very rare cases, a doctor may order a skin biopsy to confirm the disease and rule out any other possibilities.
Distinguish Lichen Planus from Condylomata Acuminata – Diagnosis
Lichen Planus is an inflammatory condition of the skin that causes redness and itching. It usually affects the skin, hair, nails, and mouth. When it appears on the genital area, it may be difficult to treat and may cause pain during intercourse. The cause of lichen planus is unknown but may be related to a decrease in immunity or a kind of allergic reaction, and some people link it to the hepatitis C virus. Lichen Planus is not contagious.
- A skin biopsy is usually the gold standard test for the confirmation of the diagnosis of lichen planus.
- Physical examination and detecting the “6 P’s,” which are: Pruritic, Polygonal, Planar, Purple papules, and Plaques, may also help doctors for diagnosis.
Distinguish Molluscum Contagiosum from Condylomata Acuminata – Diagnosis
Molluscum contagiosum is a viral infection caused by the poxvirus. It causes itchy lesions on the skin. It’s usually contagious and transmitted in wet conditions mainly.
These lesions usually don’t require treatment and may go away on their own but can take up to 2 years. Treatment may be needed when these lesions appear on genital areas.
- Diagnosing molluscum contagiosum is usually by physical appearance under a dermatoscope.
- Skin biopsy is rarely needed and only needed if the diagnosis is not clear.
Distinguish Herpes Simplex Virus (HSV) from Condylomata Acuminata – Diagnosis
Herpes simplex virus is a common viral infection that causes painful, itchy lesions on the skin, mainly oral mucosa and genital areas. Up to 60% of people worldwide get infected; it’s easily transmitted by direct contact.
- A swab from the lesion may be taken for viral culture to confirm the infection.
- A blood test for the detection of HSV antibodies (IGM) can be used.
Distinguish Buschke-Lowenstein Tumor from Condylomata Acuminata – Diagnosis
Buschke Lowenstein tumor is a rare condition characterized by an overgrowth of warts. In most cases, it’s benign and caused by the human papillomavirus. It is most commonly found in men in the genital area. In some cases, it may transform into a verrucous carcinoma.
Buschke Lowenstein tumor is a form of condylomata acuminata infection with the same characteristic cauliflower appearance. The main difference is the huge size of Buschke Lowenstein tumor and its tendency to transform into malignancy.
- In most cases, MRI is needed for the diagnosis of Buschke Lowenstein tumor and knowing the extent and size of the tumor and to rule out any metastasis.
- A biopsy may be needed to confirm the tumor as well.
“In most cases, Buschke Lowenstein tumor doesn’t cause any metastasis and can be removed surgically without the need for chemotherapy. But it does have a high recurrence rate.”
Important Red Flags in Condylomata Acuminata
Genital warts can easily be diagnosed by their appearance. In some cases, performing a pap smear is needed to rule out any cervical or vaginal changes that may be caused by the virus.
Genital warts don’t usually require treatment. You can ask your doctor for some medication if they cause some itching or pain, or you are afraid of causing an outbreak. A small surgery with local anesthetic can be performed to remove the warts as well. The virus itself doesn’t have any cure and unfortunately has a high recurrence rate.
