Contents
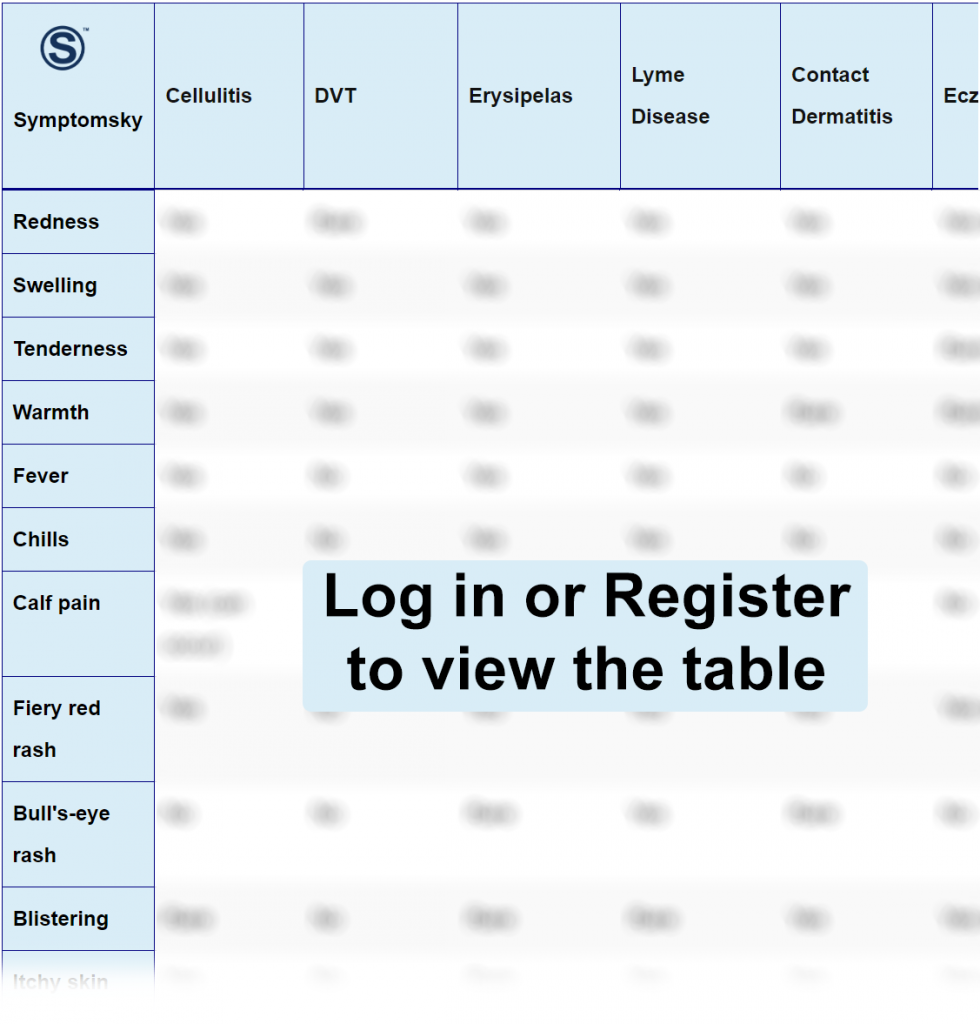
- 1 Cellulitis Differential Diagnosis Table:
- 2 How To Differentiate Cellulitis from Other Diseases
- 2.1 Distinguish DVT from Cellulitis – Diagnosis
- 2.2 Distinguish Erysipelas from Cellulitis – Diagnosis
- 2.3 Distinguish Lyme Disease from Cellulitis – Diagnosis
- 2.4 Distinguish Contact Dermatitis from Cellulitis – Diagnosis
- 2.5 Distinguish Eczema from Cellulitis – Diagnosis
- 2.6 Distinguish Lymphangitis from Cellulitis – Diagnosis
- 2.7 Distinguish Abscess from Cellulitis – Diagnosis
- 2.8 Distinguish Gangrene from Cellulitis – Diagnosis
- 2.9 Distinguish Necrotizing Fasciitis from Cellulitis – Diagnosis
- 3 Important Red Flags With Cellulitis
Cellulitis Differential Diagnosis Table:
The term cellulitis is commonly used to describe an acute bacterial non-necrotizing infection of the skin, resulting in inflammation of the deep dermis and the surrounding subcutaneous tissue. The bacteria mostly implicated include Group A Beta-hemolytic Streptococcus (Streptococcus pyogenes) and Staphylococcus aureus (often community-acquired methicillin-resistant Staphylococcus).
It is a common bacterial skin infection with 14 million cases occurring annually in the United States. Cellulitis usually follows a breach in the skin, although a portal of entry may not be obvious. The breach may involve microscopic skin changes or invasive qualities of certain bacteria.
Patients with Cellulitis usually present with the classical signs and symptoms of inflammation on the body part affected (mostly the lower extremities and rarely bilateral), and these signs include pain, warmth, a rapidly spreading or poorly demarcated area of erythema/redness, and edema/swelling. Fever and regional lymph node enlargement may occur in more serious infections.
The diagnosis of Cellulitis can be achieved clinically at the bedside, and this is done by a physical examination of the affected area for the symptoms mentioned above. Certain findings may suggest the most likely pathogen implicated, and staphylococcus is most likely if there is an underlying drainage, penetrating wound, eschar, or abscess on the site.
How To Differentiate Cellulitis from Other Diseases
Distinguish DVT from Cellulitis – Diagnosis
This is a medical condition that occurs when a blood clot forms in a deep vein; usually, it develops in the deep veins of the lower legs, the thighs, or pelvis. It can also occur in the arm.
- Similar to Cellulitis, the clinical features include; it mostly affects one limb (rarely bilateral), and the symptoms are throbbing pain in the calf or thigh when standing up or walking, leg swelling or edema, warmth, and redness over the area of the thrombosis.
- Alternately, the veins could be palpated as indurated, cordlike, tender subcutaneous venous segment, or could be occult, i.e., asymptomatic, with its primary presentation being signs of pulmonary embolism such as shortness of breath, chest pain, and cough.
Distinguish Erysipelas from Cellulitis – Diagnosis
Erysipelas is a bacterial skin infection involving the upper dermis and the superficial cutaneous lymphatic.
- Similarly to Cellulitis, it presents as tender, intensely erythematous plaques.
- The differentiating feature between Erysipelas and Cellulitis is the fact that the lesion in Erysipelas has a well-defined/demarcated margin, and high fever, chills, and malaise may follow Erysipelas.
Distinguish Lyme Disease from Cellulitis – Diagnosis
Lyme Disease is the most common vector-borne illness in the United States. It is a bacterial infection caused by the spirochete Borrelia burgdorferi and the body’s immune response to the infection. This disease is transmitted to humans via bites from infected ticks of genus Ixodes.
- In contrast to Cellulitis, the earliest signs/symptoms are those of a flu, such as fever, chills, malaise, arthralgia, headache, and localized tender adenopathy. It also presents with Erythema migrans in the course of the illness.
Distinguish Contact Dermatitis from Cellulitis – Diagnosis
Contact dermatitis is an allergic skin condition caused by exposure of the skin to irritants. This irritant could be cosmetics, fragrances, jewelry, plants, or even contact with another human being’s skin or body fluid.
- Similarly to Cellulitis, contact dermatitis presents with swelling, a burning sensation/tenderness, and redness around the affected area.
- In contrast to Cellulitis, the clinical features of contact dermatitis also include an itchy rash, dry cracked scaly skin, bumps and blisters, and leathery patches that are darker than usual, typically on black or brown skin.
Distinguish Eczema from Cellulitis – Diagnosis
Eczema is also called atopic dermatitis. This entails that it is an inflammatory skin condition that causes the skin to become dry, itchy, and bumpy, thereby weakening the skin’s barrier function responsible for skin moisture retention and protection from external elements.
- Generally, symptoms of Eczema include dry skin, itchy skin, skin rash, bumps, flaky, scaly, or crusty skin, and swelling.
- The above symptoms can affect almost all parts of the body, unlike cellulitis, which is more common in the lower extremities.
- There is a greater chance of being diagnosed with eczema if an individual has a family history of dermatitis, allergies, hay fever, or asthma.
Distinguish Lymphangitis from Cellulitis – Diagnosis
Lymphangitis is an infection and inflammation of the lymph channels/lymph vessels. It occurs as a result of an infection at a site distal to the channel. If there’s an infection in the hand, the inflammation will be towards the arm. Although skin infections are the most common cause, the invading microbe can also get into the channel through skin abrasions or a wound.
- Similarly to cellulitis, the infection is usually caused by Group A beta-hemolytic Streptococci, followed by Staphylococcus aureus.
- The disease manifests as linear red streaks on the skin that are tender and warm, from the site of the infection to the regional lymph node. Patients may also present with fever, chills, and malaise.
- Lymphangitis can occur following cellulitis.
Distinguish Abscess from Cellulitis – Diagnosis
This condition develops when an infection causes a pocket/collection of pus in a particular part of the body, and the name follows, for example, skin abscess when it is on the skin. It could also affect the mouth or inside the internal organs or cavities of the body.
- The signs and symptoms depend on the body part/location affected, but generally, the symptoms include pain in/around the area, swelling, discoloration around the edges, presence of a hard or soft lump, pus-filled center, fever, fatigue, and chills.
- An abscess could be a complication of delayed treatment of cellulitis.
Distinguish Gangrene from Cellulitis – Diagnosis
Gangrene is a medical condition that results from a deficient supply of oxygen-rich blood to a particular body part with the potential to cause tissue death if urgent treatment/care is not instituted. It mostly affects the hands and the feet, although it could possibly affect the internal organs, in which case it is called internal gangrene.
- Symptoms on the skin include; blisters, bluish skin discoloration, ulcers, pain, etc.
- If there is internal gangrene, the symptoms would include; fever, hypotension, nausea and vomiting, dyspnea, and tachycardia.
- Unlike Cellulitis, gangrene also affects internal organs and muscles.
Distinguish Necrotizing Fasciitis from Cellulitis – Diagnosis
Necrotizing Fasciitis, also known as flesh-eating disease, is a rare but serious bacterial infection. It can result from a secondary bacterial infection of a wound, and it spreads very rapidly through deep tissues in the body.
Important Red Flags With Cellulitis
Cellulitis is a painful bacterial infection of the deeper layers of the skin and surrounding soft tissues. A number of diseases with varying severity ranging from mild to severe can mimic its symptoms, and inappropriate treatment could lead to complications such as abscess formations, lymphangitis, etc. As such, a proper diagnosis needs to be made on the patient’s arrival at the health facility to ensure timely and adequate treatment.
A clear understanding and proper physical examination will reduce the chances of misdiagnosing Erysipelas, which affects only the superficial dermis and superficial lymphatic channel.
