Contents
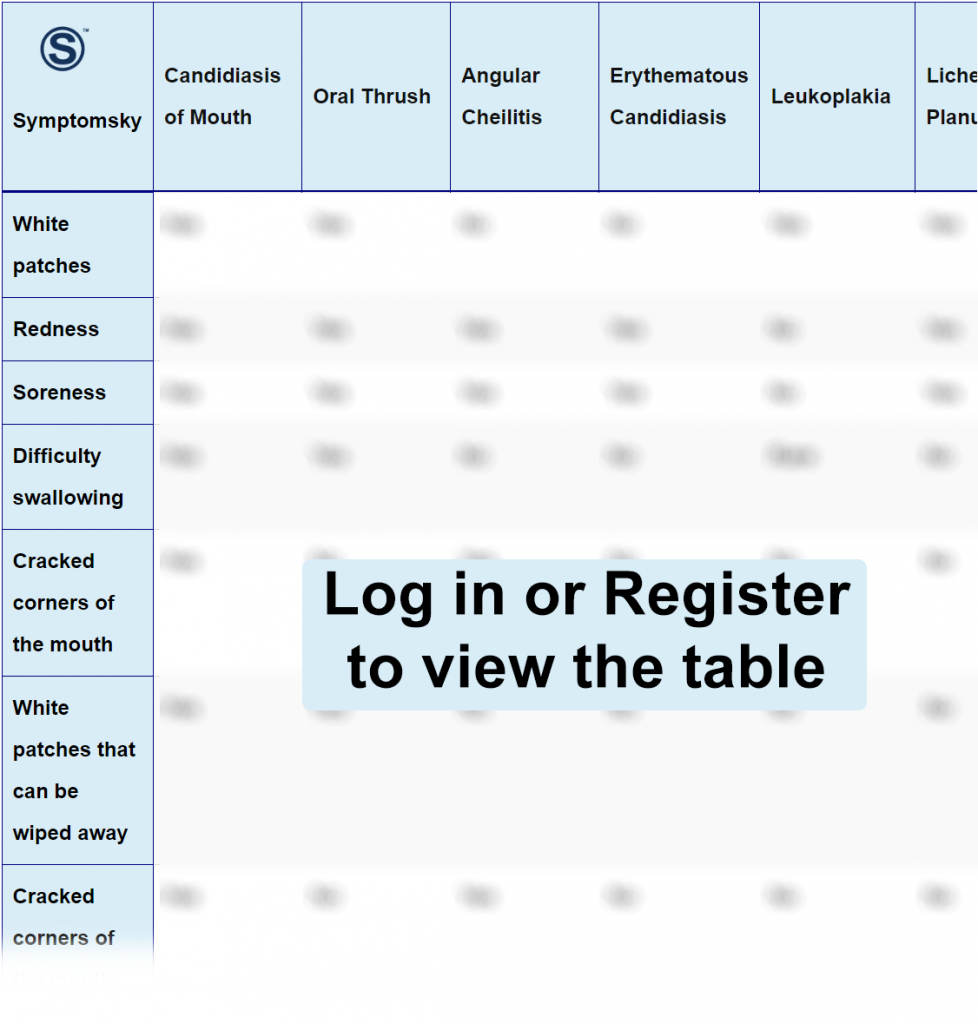
- 1 Candidiasis of Mouth Differential Diagnosis Table:
- 2 How to Distinguish Oral Candidiasis from Other Diseases
- 2.1 Distinguish Oral Thrush from Oral Candidiasis – Diagnosis
- 2.2 Distinguish Angular Cheilitis from Oral Candidiasis – Diagnosis
- 2.3 Distinguish Erythematous Candidiasis from Oral Candidiasis – Diagnosis
- 2.4 Distinguish Leukoplakia from Oral Candidiasis – Diagnosis
- 2.5 Distinguish Lichen Planus from Oral Candidiasis – Diagnosis
- 2.6 Distinguish Aphthous Stomatitis from Oral Candidiasis – Diagnosis
- 2.7 Distinguish Herpes Labialis from Oral Candidiasis – Diagnosis
- 2.8 Distinguish Herpes Simplex Virus Infection from Oral Candidiasis – Diagnosis
- 2.9 Distinguish Herpes Gingivostomatitis from Oral Candidiasis – Diagnosis
- 2.10 Distinguish Angioedema from Oral Candidiasis – Diagnosis
- 3 Oral Candidiasis Management and Treatment
Candidiasis of Mouth Differential Diagnosis Table:
Oral candidiasis is a yeast infection affecting the oral cavity, usually due to local or systemic immunosuppression. Oral candidiasis appears as white lesions, which have a “cottage cheese” appearance. White lesions can be scraped off easily by gauze, leaving a red inflamed mucosal surface behind.
Lesions are asymptomatic, yet, if symptomatic, patients experience a burning sensation, difficulty in eating and swallowing, oral bleeding, a sore tongue, cracks at the mouth corners, and disruption in taste buds. Along with clinical findings and risk factors assessment, it can also be diagnosed by potassium hydroxide culture test and microscopic examination.
Oral candidiasis has predisposing factors that can be managed for prevention. This can be done by proper patient education as for steroid inhalers patients should be educated to rinse their mouth after each application, patients also should have proper nutrition as oral candidiasis is associated with iron and vitamins deficiency, in addition to proper dental hygiene and limiting sugar intake (as sugar is favorable flora for candida).
How to Distinguish Oral Candidiasis from Other Diseases
Distinguish Oral Thrush from Oral Candidiasis – Diagnosis
- Oral Thrush is limited to the oral cavity, while oral candidiasis involves cracks around the mouth.
“Microscopic examination and culture are used for differentiation.”
Distinguish Angular Cheilitis from Oral Candidiasis – Diagnosis
- Angular cheilitis involves red inflamed painful patches of skin at the labial commissures, while Oral candidiasis involves white patches in the oral cavity.
- Angular cheilitis is limited to angles of the mouth, while oral candidiasis involves angles of the mouth along with the oral cavity.
“Clinical findings in addition to bacterial or Candida culture are used for differentiation.”
Distinguish Erythematous Candidiasis from Oral Candidiasis – Diagnosis
- Erythematous candidiasis is associated with prolonged ingestion of broad-spectrum antibiotics, while oral candidiasis is not associated with antibiotic ingestion.
- Erythematous candidiasis is red inflamed lesions only found at the dorsum of the tongue, while oral candidiasis is white patches affecting the oral cavity.
“Clinical and microscopic examination are used for differentiation.”
Distinguish Leukoplakia from Oral Candidiasis – Diagnosis
- Leukoplakia is white thick patches that cannot be scraped off, unlike oral candidiasis where white patches can be scraped off easily.
- Leukoplakia is asymptomatic, while oral candidiasis has symptoms such as a burning sensation.
“Biopsy is used for differentiation, along with clinical examination.”
Distinguish Lichen Planus from Oral Candidiasis – Diagnosis
- Lichen Planus has a distinctive lattice-like network of white lines, while oral candidiasis presents as white patches.
“Dermascope and microscopic examination are used for differentiation.”
Distinguish Aphthous Stomatitis from Oral Candidiasis – Diagnosis
- Aphthous stomatitis involves ulcers without white patches, while oral candidiasis does not involve ulcers, and white patches are a crucial clinical finding.
Distinguish Herpes Labialis from Oral Candidiasis – Diagnosis
- Herpes labialis is a viral infection, while oral candidiasis is a fungal infection.
- Herpes labialis affects orolabial tissue without mucosal involvement, while oral candidiasis affects the oral mucosal cavity.
“PCR, culture, and DFA assay are used for differentiation.”
Distinguish Herpes Simplex Virus Infection from Oral Candidiasis – Diagnosis
- Herpes simplex virus affects orolabial and genital areas, while oral candidiasis affects the oral mucosal cavity.
- Herpes simplex virus is associated with painful blistering without mucosal involvement, unlike oral candidiasis where blistering is absent and limited to the oral cavity.
“HSV-1 serology, PCR, culture, and DFA assay are used for differentiation.”
Distinguish Herpes Gingivostomatitis from Oral Candidiasis – Diagnosis
- Herpes gingivostomatitis appears as oral vesicles and ulcerative lesions, while oral candidiasis appears as white patches.
“Direct immunofluorescent examination and tissue culture are used for differentiation.”
Distinguish Angioedema from Oral Candidiasis – Diagnosis
Angioedema is a hypersensitivity reaction due to allergen exposure.
- Angioedema involves the skin (urticaria and pruritus) and respiratory system (bronchospasm), while oral candidiasis does not involve skin or respiratory manifestations.
“Blood tests are used for differentiation.”
Oral Candidiasis Management and Treatment
Oral candidiasis usually does not have complications but in severe immunocompromised patients and failure of treatment, pharyngeal involvement may be present, which is experienced as respiratory distress and dysphagia.
Oral candidiasis can be resolved by proper dental hygiene and topical antifungals such as nystatin, miconazole, clotrimazole, and ketoconazole. If the condition is sustained, a systemic antifungal is considered. In cases of moderate to severe oral candidiasis, fluconazole is considered.
