Contents
- 1 Benign Essential Hypertension Differential Diagnosis Table:
- 2 How to Distinguish Benign Essential Hypertension from Other Diseases
- 2.1 Distinguish Pheochromocytoma from Benign Essential Hypertension – Diagnosis
- 2.2 Distinguish Renal Artery Stenosis from Benign Essential Hypertension – Diagnosis
- 2.3 Distinguish Hyperthyroidism from Benign Essential Hypertension – Diagnosis
- 2.4 Distinguish Cushing Syndrome from Benign Essential Hypertension – Diagnosis
- 2.5 Distinguish Sleep Apnea from Benign Essential Hypertension – Diagnosis
- 2.6 Distinguish Primary Aldosteronism from Benign Essential Hypertension – Diagnosis
- 2.7 Distinguish Coarctation of Aorta from Benign Essential Hypertension – Diagnosis
- 2.8 Distinguish Conn’s Syndrome from Benign Essential Hypertension – Diagnosis
- 3 Management and Treatment of Benign Essential Hypertension
Benign Essential Hypertension Differential Diagnosis Table:
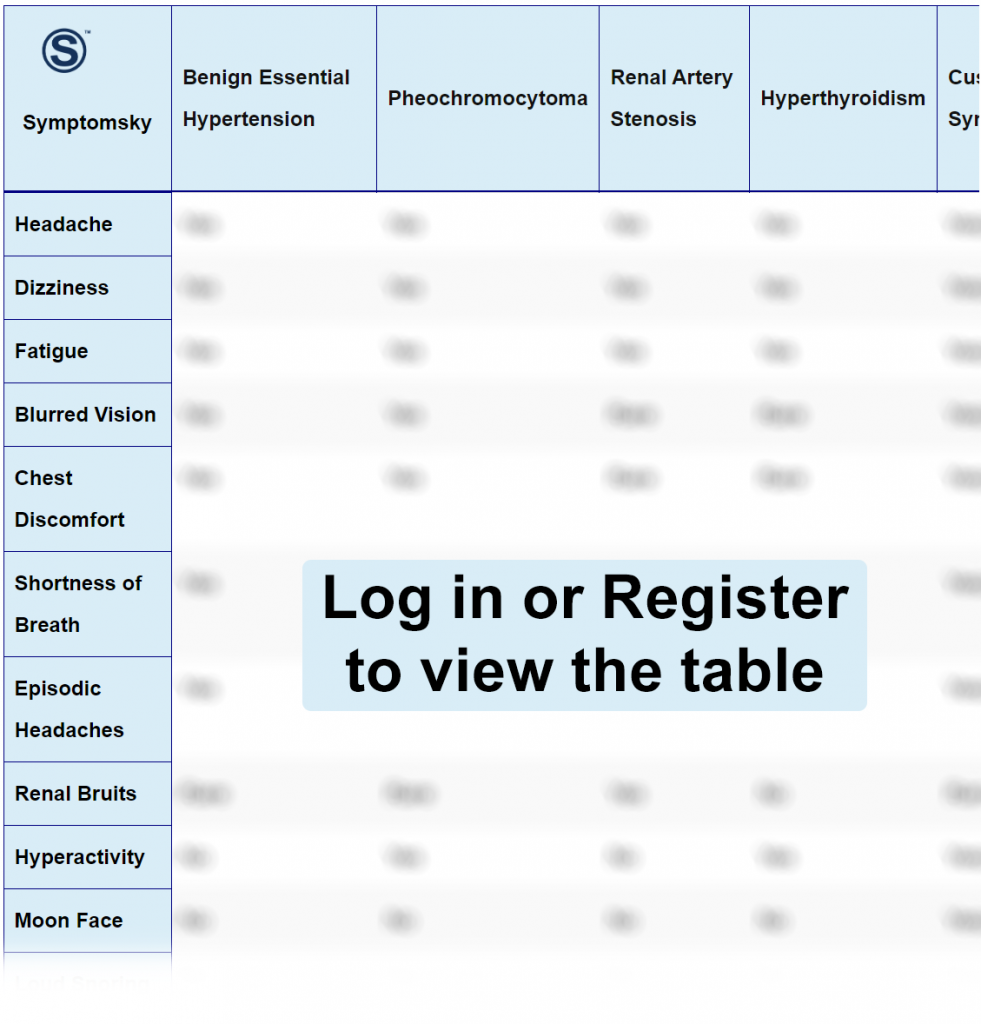
Benign Essential Hypertension is chronic mild to moderately persistent elevation in arterial pressure with no underlying cause (idiopathic). Overall increased in afterload and total peripheral resistance. The diagnosis of benign essential hypertension is two measurements at two separate timings: Systolic Blood pressure more than 130mmHg and Diastolic more than 80mmHg. Benign hypertension can be asymptomatic to mild symptoms such as headache, dizziness, nausea, and fatigue.
How to Distinguish Benign Essential Hypertension from Other Diseases
Distinguish Pheochromocytoma from Benign Essential Hypertension – Diagnosis
Pheochromocytoma is a tumor from the adrenal gland, causing excessive secretion of catecholamines and activation of the sympathetic nervous system.
- Pheochromocytoma includes excessive sweating and anxiety, but Benign Essential hypertension has mild symptoms such as headache, nausea, and fatigue.
- Pheochromocytoma is resistant to medications, while Benign essential hypertension is affected by medications.
- Sudden hypertension attacks and tachycardia are accompanied with pheochromocytoma, but absent in benign essential hypertension.
“Plasma and urine analysis are used for differentiation.”
Distinguish Renal Artery Stenosis from Benign Essential Hypertension – Diagnosis
Renal artery stenosis is a condition of narrowing or blockage of the renal artery.
- Renal artery stenosis is accompanied with resistant severe hypertension, but benign essential hypertension is mild to moderate hypertension and favorable for medications.
- Renal artery stenosis is characterized by renal bruit (whooshing sound), but renal bruit is absent in benign essential hypertension.
“Plasma and urine analysis are used for differentiation, in addition to Renal arteriography.”
Distinguish Hyperthyroidism from Benign Essential Hypertension – Diagnosis
Hyperthyroidism is dysfunction of the thyroid gland producing an increased amount of thyroid hormones.
- Hyperthyroidism is characterized by weight loss, increased appetite, and heat intolerance, while benign essential hypertension does not include weight loss, increased appetite, or heat intolerance.
- Hyperthyroidism causes tremors, while tremors are absent in benign essential hypertension.
“Lab tests (TSH, T3, and Free T4) are used for diagnosis.”
Distinguish Cushing Syndrome from Benign Essential Hypertension – Diagnosis
Cushing syndrome is a group of symptoms that arise from prolonged exposure of the body to high levels of cortisol.
- Cushing syndrome patients are characterized by buffalo torso (deposition of fat around the belly), moon face, paper-thin skin, and thin arms & legs, but this appearance is absent in benign essential hypertension.
- Cushing syndrome includes abnormal excessive sweating, which is absent in Benign Essential Hypertension.
“Late-night salivary cortisol and 24 hours free cortisol urine samples are used for differentiation.”
Distinguish Sleep Apnea from Benign Essential Hypertension – Diagnosis
Sleep apnea is a temporary episode of partial blockage of the airway (hypopnea) or complete blockage of the airway (apnea) during sleep
- Sleep apnea is associated with loud snoring, which is absent in benign essential hypertension.
- Sleep apnea includes episodes of gasping and choking during sleep, but benign essential hypertension does not include episodes of gasping and choking during sleep.
“In-laboratory/in-home-polysomnogram is used for differentiation.”.
Distinguish Primary Aldosteronism from Benign Essential Hypertension – Diagnosis
- Primary aldosteronism is a rare hormonal disruption that results in increased aldosterone production from the adrenal gland.
- Primary aldosteronism causes hypokalemia, but potassium levels are normal in benign essential hypertension.
- Primary aldosteronism has resistant hypertension to medications, unlike Benign essential hypertension is affected by medications.
“Aldosterone-to-Renin plasma ratio is used for differentiation.”
Distinguish Coarctation of Aorta from Benign Essential Hypertension – Diagnosis
Coarctation of the aorta, narrowing causing upper extremities hypertension, is presented in neonates.
- Coarctation of Aorta has hypertension in upper extremities, but benign essential hypertension is hypertension in all body.
- Coarctation of Aorta is characterized by the absence of femoral pulses, while in benign essential hypertension femoral pulses are normal.
- Coarctation of Aorta is associated with a gallop sound upon auscultation, which is absent in Benign essential hypertension.
“Imaging such as EKG is used for differentiation.”
Distinguish Conn’s Syndrome from Benign Essential Hypertension – Diagnosis
Conn’s syndrome is an adrenal tumor producing excessive aldosterone.
- Conn’s syndrome includes frequent urination and thirst, while these symptoms are absent in benign essential hypertension.
“Aldosterone-to-Renin plasma ratio is used for differentiation.”.
Management and Treatment of Benign Essential Hypertension
Including lifestyle changes such as salt restriction, smoking cessation, weight, and increased physical activity. Pharmacological interventions take place along with lifestyle changes in patients with blood pressure persistent over 140/90mmHg, including diuretics, angiotensin-converting enzyme inhibitors (ACEi), calcium channel blockers, beta-blockers, and angiotensin receptor blockers (ARBs).
