Contents
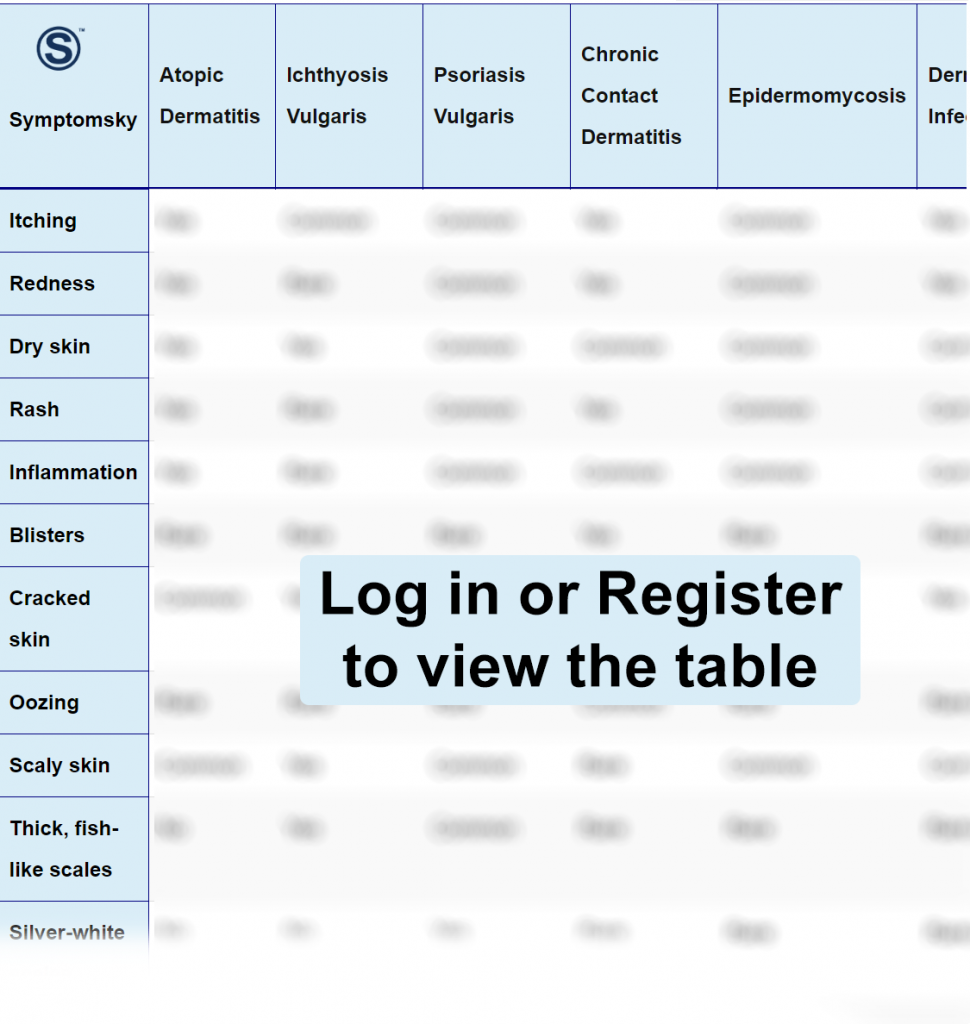
- 1 Atopic Dermatitis Differential Diagnosis Table:
- 2 How to Distinguish Atopic Dermatitis from Other Diseases
- 2.1 How to Distinguish Ichthyosis Vulgaris from Atopic Dermatitis – Diagnosis
- 2.2 How to Distinguish Psoriasis Vulgaris from Atopic Dermatitis – Diagnosis
- 2.3 How to Distinguish Chronic Contact Dermatitis from Atopic Dermatitis – Diagnosis
- 2.4 How to Distinguish Epidermomycosis from Atopic Dermatitis – Diagnosis
- 2.5 How to Distinguish Dermatophyte Infection from Atopic Dermatitis – Diagnosis
- 2.6 How to Distinguish Seborrheic Dermatitis from Atopic Dermatitis – Diagnosis
- 2.7 How to Distinguish Scabies from Atopic Dermatitis – Diagnosis
- 2.8 How to Distinguish Neurodermatitis from Atopic Dermatitis – Diagnosis
- 2.9 How to Distinguish Immunodeficiency Disorders from Atopic Dermatitis – Diagnosis
- 3 Common Red Flags with Atopic Dermatitis
Atopic Dermatitis Differential Diagnosis Table:
Atopic Dermatitis is an inflammatory skin disease that consists of intense pruritus and dry skin; it has a chronic course. This condition does not affect a particular group since it can present at any age. It should be noted that this condition is more frequent in children; in fact, most of the cases occur during the first year of life.
The incidence of this condition has increased over the last years, especially in industrialized countries. This disease produces a significant impact on the patient and family’s life since, as described before, it affects infants.
Atopic dermatitis elementary lesion is a very poorly delimited eczema with intense pruritus.
How to Distinguish Atopic Dermatitis from Other Diseases
How to Distinguish Ichthyosis Vulgaris from Atopic Dermatitis – Diagnosis
Ichthyosis is a dominant autosomal disease.
- Ichthyosis vulgaris is an inherited condition, unlike atopic dermatitis, that has an important hereditary component. However, it is a multifactorial disease; it’s not as strong as ichthyosis.
- Ichthyosis vulgaris is characterized by very dry skin with scales causing crusts, while atopic dermatitis is a very poorly delimited erythematous eczema with intense pruritus.
How to Distinguish Psoriasis Vulgaris from Atopic Dermatitis – Diagnosis
Psoriasis is an inherited condition.
- Psoriasis vulgaris presents redness, parakeratosis on top of a highly inflammatory-based and scaly skin, while atopic dermatitis is a very poorly delimited erythematous eczema with intense pruritus.
- Psoriasis vulgaris is an inherited condition, unlike atopic dermatitis, that has an important hereditary component. However, it is a multifactorial disease; it’s not as strong as psoriasis.
How to Distinguish Chronic Contact Dermatitis from Atopic Dermatitis – Diagnosis
Chronic contact dermatitis is the inflammation of the skin caused by the direct contact of some irritants.
- Chronic contact dermatitis usually relates to non-allergic irritating substances, while atopic dermatitis is linked to allergic substances.
- Chronic contact dermatitis lesions are very delimited in the area where the patient was exposed to the substance, unlike atopic dermatitis where the lesions can be present all over the skin.
- Chronic contact dermatitis has numerous small blisters and pustules, while atopic dermatitis does not present these characteristics in its clinical presentation.
How to Distinguish Epidermomycosis from Atopic Dermatitis – Diagnosis
Epidermomycosis is a fungal condition.
- Epidermomycosis presents a ringworm with active and flaky edges, while atopic dermatitis is a very poorly delimited erythematous eczema with intense pruritus.
- Epidermomycosis is a fungal infection, unlike atopic dermatitis, which is an inflammatory skin condition.
How to Distinguish Dermatophyte Infection from Atopic Dermatitis – Diagnosis
Dermatophyte infection is a superficial infection.
- The dermatophytes require keratin to grow; therefore, the affected areas will be places containing keratin such as hair, nails, and skin, unlike atopic dermatitis which can appear anywhere.
- Patients with dermatophyte infection can also present irregular alopecia, while in atopic dermatitis, it is very rare.
- Dermatophyte infection is caused by a fungus, while atopic dermatitis is an inflammatory condition.
How to Distinguish Seborrheic Dermatitis from Atopic Dermatitis – Diagnosis
Is a chronic inflammation.
- Seborrheic dermatitis usually occurs in the first weeks of life, unlike atopic dermatitis which tends to appear after 2 months of life.
- Seborrheic dermatitis presents yellowish gray scales, redness in areas saturated in sebaceous content such as scalp, eyebrows, face, and inguinal region while atopic dermatitis is a very poorly delimited erythematous eczema with intense pruritus.
How to Distinguish Scabies from Atopic Dermatitis – Diagnosis
Scabies is an itchy condition caused by parasites.
- Scabies is characterized by the appearance of linear lesions followed by pearly vesicles filled with fluid in the affected region, while atopic dermatitis is a very poorly delimited erythematous eczema with intense pruritus.
- In Scabies, the pruritus worsens at night, unlike atopic dermatitis, where pruritus does not have a defined schedule.
- Scabies affects everyone who lives with the patient affected, especially if they share clothes or sleep together, and it is important that all of them carry out the treatment, while atopic dermatitis is not contagious, so it does not affect anyone else in the house.
How to Distinguish Neurodermatitis from Atopic Dermatitis – Diagnosis
Neurodermatitis is a skin condition that causes itching.
- Neurodermatitis, unlike Atopic Dermatitis, is limited to specific patches. This condition generates intense itching to the patient, causing a lot of wounds that will develop scars formed on a thick layer of rough texture.
- The most common form of neurodermatitis is called lichen simplex chronicus, which presents scaly, thick, patchy areas, while atopic dermatitis is a very poorly delimited erythematous eczema with intense pruritus.
How to Distinguish Immunodeficiency Disorders from Atopic Dermatitis – Diagnosis
Primary immunodeficiencies are a group of genetic diseases in which there is an alteration in the mechanisms that regulate the immune response.
- In combined immunodeficiencies, unlike Atopic Dermatitis, the thymus may be small or absent. Children have serious, unusually life-threatening recurrent infections, such as pneumonia, diarrhea, and sepsis. They also have opportunistic germ infections that cause weight and height alterations.
- In immunodeficiencies combined with syndrome characteristics, unlike Atopic Dermatitis patients, have cardiac malformations such as tetralogy of Fallot, seizures, as well as facial features like cleft palate lip. These patients suffer from nervous system conditions that are manifested by disturbances while walking and telangiectasis. They also present recurrent respiratory and gastrointestinal infections.
- In immunodeficiencies of antibodies, unlike Atopic Dermatitis, usually occur during pregnancy so these patients will have low levels of IgG and IgA up to three or four years of age. They may present recurrent respiratory and gastrointestinal infections. These patients have a greater predisposition to autoimmune diseases and cancer.
- In immunodeficiencies with immune dysregulation, unlike Atopic Dermatitis, they present fever associated with abnormal growth of certain organs such as the liver, spleen, and lymph nodes.
- In phagocyte defects, unlike Atopic Dermatitis, a decrease in the number of neutrophils can be found in the laboratory results. These patients usually have inflammations of the gingival and oral mucosa; also, they have recurrent infections as well as the presence of abscesses on the skin in other internal organs such as the liver and lung. In these patients, chronic granulomatous disease may occur, which has the presence of ganglion growths at the site where the BCG vaccine is placed. Also, these patients often have pneumonia caused by fungi or bacterial agents.
- In innate immunity defects, unlike Atopic Dermatitis, patients may present a predisposition to viral or fungal infections as well as the abnormal presence of warts on the body.
- In self-inflammatory disorders, unlike Atopic Dermatitis, they are characterized by recurrent periodic fevers in which the immune system acts with a hyper response. The main symptoms are fever without a certain cause, as well as joint pain and lymphadenopathies.
- Deficiencies of the complement, unlike Atopic Dermatitis, may present pneumonia and meningitis as well as the presence of kidney diseases, arthritis, etc.
How to Distinguish Systemic Disorders from Atopic Dermatitis – Diagnosis
We must suspect a metabolic disease when there is an infant with eczema that does not respond to the usual treatments for AD and has continuous infections.
- Patients with phenylketonuria, unlike Atopic Dermatitis, may develop intellectual disabilities, developmental delay, eruptions, psychiatric disorders, social and emotional behavioral problems, as well as moisture odor in the breath and urine due to the accumulation of phenylalanine in the body.
Common Red Flags with Atopic Dermatitis
It is important to know that this condition is a chronic disease, the most frequent in childhood. It is very important to educate the patient’s family since the nature of this disease will affect their quality of life. Understanding that this disease does not have a healing treatment, it will not improve over the years, it is very important that the patient adheres to treatment and follow-ups. Explain to the patient to avoid exacerbations, avoid situations where the cutaneous barrier is compromised such as not applying moisturizing creams after taking a bath, using strongly scented detergents for clothes.
There are diagnostic criteria for AD, the most common is the Hanifin and Rajka’s criteria; they divide it into major and minor criteria. Major criteria: Presence of 3 or more of these qualities: Pruritus, typical distribution lesions lichenification in flexures (adults), face affected (children and young), family history. Minor criteria: Presence of 3 or more of these qualities: Xerosis, onset of early age, elevated serical IgE, intolerance to organic solvents, frequent dermatitis (hands and foot).
In relation to the genesis of this condition, many factors are related, which are:
Genetic predisposition: There is no specific number of gene mutations that produce this unleashed inflammation of the cutaneous barrier. Among all these genes related to this condition, the best-known is the filaggrin gene; it manifests when there is an allergic family history as well as the coexistence of any other allergic diseases such as asthma, rhinitis. This factor has a lot of impact because there is a 60% probability that the child suffers from AD if one of the parents possesses it. A greater risk has been associated if the mother is the one.
Unstabilized cutaneous barrier: This condition involves having dry and permeable skin, making an easier entry for different allergens from the environment through the skin.
