Contents
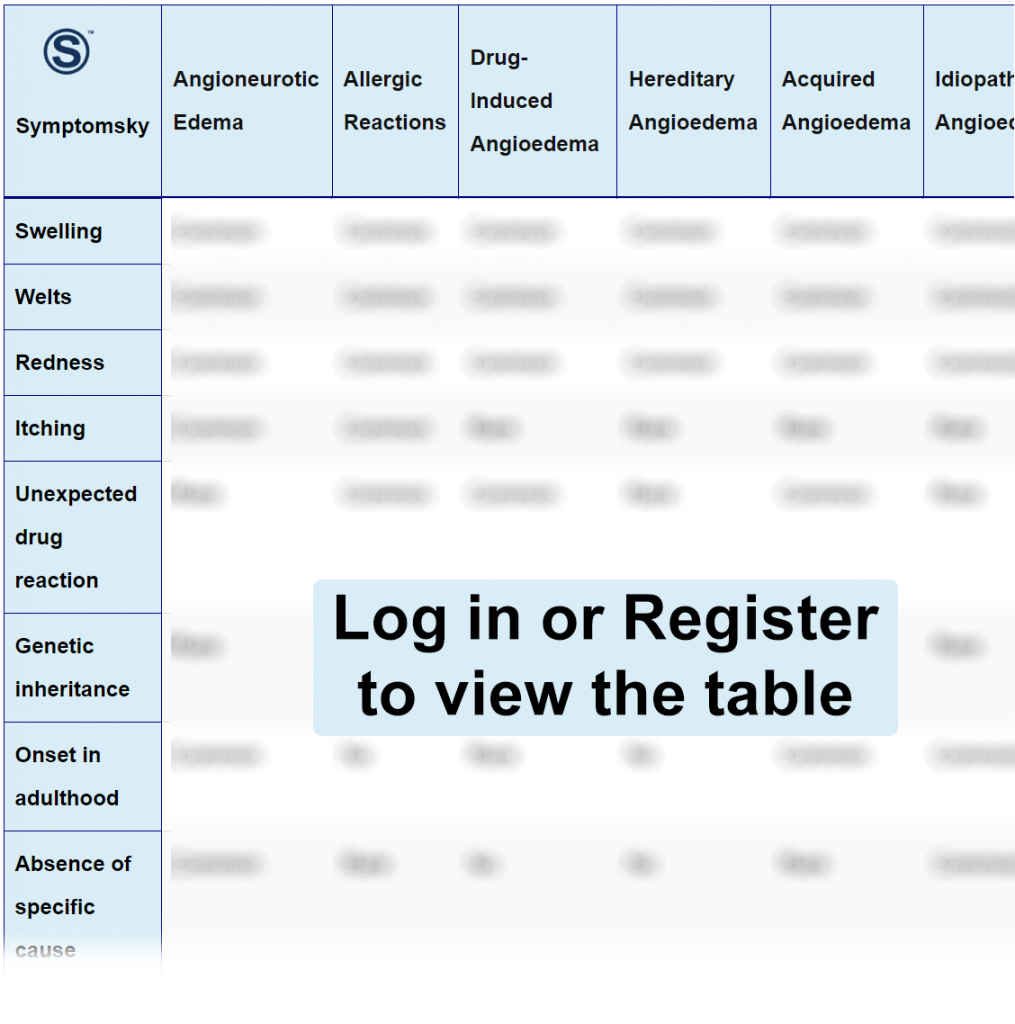
- 1 Angioneurotic Edema Differential Diagnosis Table:
- 2 How to Distinguish Angioneurotic Edema from Other Diseases
- 2.1 Distinguish Allergic Reactions from Angioneurotic Edema – Diagnosis
- 2.2 Distinguish Drug-Induced Angioedema from Angioneurotic Edema – Diagnosis
- 2.3 Distinguish Hereditary Angioedema from Angioneurotic Edema – Diagnosis
- 2.4 Distinguish Acquired Angioedema from Angioneurotic Edema – Diagnosis
- 2.5 Distinguish Idiopathic Angioedema from Angioneurotic Edema – Diagnosis
- 3 Important Red Flags in Angioneurotic Edema
Angioneurotic Edema Differential Diagnosis Table:
Angioneurotic edema, also known as angioedema, is a reaction that usually results in swelling and inflammation in tissue and layers under the skin (Deep dermal layers). This usually appears as swelling in the face, eyelids, lips, and tongue. In severe cases, swelling of the neck may occur, which may result in a life-threatening condition and require immediate medical management.
Angioedema may result from a number of causes: genetics, hypersensitivity, and sometimes it’s idiopathic. Treatment varies according to severity.
There are two types of angioedema: Histamine-mediated, which results in itching, unlike bradykinin-mediated angioedema, which doesn’t cause itching or urticaria.
Diagnosis of angioedema mainly depends on physical examination; blood tests (CRP, ESR) can also be used for confirmation of the disease and to monitor prognosis and response to treatment.
How to Distinguish Angioneurotic Edema from Other Diseases
Distinguish Allergic Reactions from Angioneurotic Edema – Diagnosis
Allergic reactions can happen when the body triggers an immune reaction towards a specific substance, the body usually mistakes this item as a foreign body and causes a series of immune and inflammatory responses, causing symptoms that can range from very mild itch or rash to severe allergic reactions.
- Skin prick test is the common diagnostic test for allergic reactions; it’s a thin needle that contains possible allergens to test for a hypersensitivity reaction.
- Blood tests to check for IgE to identify immune response inside the body.
“The major difference between angioneurotic edema and allergic reaction is that in angioedema, the inflammation is in tissue and layers under the skin while in allergic reaction, the swelling and inflammation are mainly in the skin surface itself.“
Distinguish Drug-Induced Angioedema from Angioneurotic Edema – Diagnosis
Drug-induced angioedema is an allergic, inflammatory reaction to a specific drug; it usually results in the same symptoms of angioedema but in this case, the cause is known to be from a drug. The most common drugs to cause angioedema are ACE inhibitors; this is due to the buildup of bradykinin leading to swelling and inflammation in tissue and submucosal layer.
- Diagnosis is based on clinical presentation and detailed patient history, especially drugs taken in the last 72 hours.
- Blood tests to detect inflammatory markers like CRP; other markers like low levels of C4 can help in the diagnosis of angioedema.
“Diagnosis of drug-induced angioedema is mainly based on clinical presentation and discontinuation of the suspected offending agent; if resolution of symptoms occurred with no further recurrence, then diagnosis is confirmed.”
Distinguish Hereditary Angioedema from Angioneurotic Edema – Diagnosis
Hereditary angioedema is a genetic condition that occurs due to deficiency in C1-inhibitor protein; usually, symptoms appear from childhood leading to attacks of angioedema once or twice weekly. The severity of symptoms usually depends on how low the level of C1-inhibitor protein is. In this type of angioedema, itching and urticaria do not occur.
- Diagnosis of Hereditary angioedema mainly depends on checking C1-inhibitor protein deficiency; this can confirm diagnosis.
“The major difference between hereditary angioedema and other types of angioedema is the level of C1 inhibitor protein, which is usually normal in other conditions having other specific causes.”
Distinguish Acquired Angioedema from Angioneurotic Edema – Diagnosis
Acquired angioedema is a condition in which there’s a dysfunction in C1-inhibitor protein. This can happen because of consumption or inactivation of the protein or, in some cases, maybe because of a disease or a tumor. Acquired and hereditary angioedema have the same manifestation and symptoms. The only difference is that in acquired angioedema, symptoms usually occur during adulthood.
- Diagnosis of acquired angioedema although depends on checking the level of C1-inhibitor protein.
- Measure of other complement levels like C4, which is common to be low in conditions of angioedema.
Distinguish Idiopathic Angioedema from Angioneurotic Edema – Diagnosis
Idiopathic angioedema means that there’s no specific cause for angioedema; some link it to anxiety or stress conditions. The challenging part in this condition is that there’s no known underlying cause, so the treatment mainly aims to control symptoms.
- Clinical presentation and detailed patient medical and drug history are important.
- Blood tests to check for IgE, to see if the underlying cause is hypersensitivity-related.
- Checking the level of C1 inhibitor protein, to see if it’s an acquired or hereditary type of angioedema.
- Checking other levels of complement like C4, since it’s usually low in angioedema.
“Since idiopathic angioedema usually has no specific cause, diagnosis is inclusive to determine any underlying condition.”
Important Red Flags in Angioneurotic Edema
Angioneurotic edema can vary in severity from a mild condition that can be easily treated by some antihistaminic medication and cortisone to a very severe condition requiring medical intervention and emergency department.
The most important red flag in angioedema is the presence of neck and tongue swelling; this can lead to a decrease in oxygen saturation and make it difficult to breathe, which may require intubation in some severe cases. So it’s important to not let the condition progress.
A very low level of C1 inhibitor protein or complete lack of the enzyme reflects that the condition is severe and requires continuous monitoring and follow-up.
