Contents
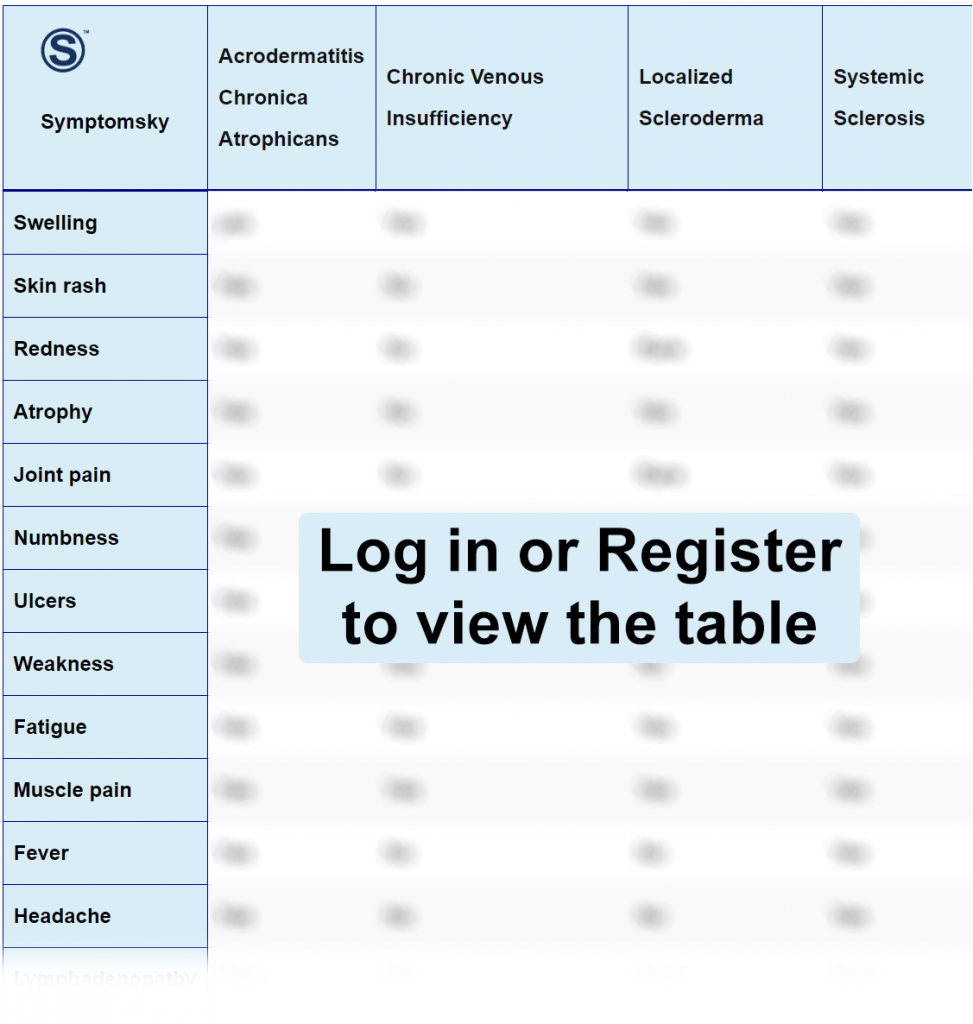
- 1 Acrodermatitis Chronica Atrophicans Differential Diagnosis Table:
- 2 How To Distinguish Acrodermatitis Chronica Atrophicans from Other Diseases
- 2.1 Distinguish Chronic Venous Insufficiency from ACA – Diagnosis
- 2.2 Distinguish Localized Scleroderma from ACA – Diagnosis
- 2.3 Distinguish Systemic Sclerosis from ACA – Diagnosis
- 2.4 Distinguish Frostbite from ACA – Diagnosis
- 2.5 Distinguish Erysipelas from ACA – Diagnosis
- 2.6 Distinguish Superficial Thrombophlebitis from ACA – Diagnosis
- 2.7 Distinguish Erysipeloid from ACA – Diagnosis
- 3 HOW TO PROTECT FROM ACA
Acrodermatitis Chronica Atrophicans Differential Diagnosis Table:
Acrodermatitis chronica atrophicans is the most common chronic and late manifestation of Lyme borreliosis. ACA mainly results from untreated bacterial infection with B. afzelii. It shows a cell-mediated immune response against Borrelia with the presence of CD3+ and CD4+ cells in the dermal infiltrates.
It causes damage to connective tissue and collagen, which leads to dermal atrophy and fibrosis. It is difficult to diagnose because of its varying clinical manifestation. It shows biphasic presentation; initially, it shows bluish-red lesions superimposed on dull and swollen skin, then it progresses into “cigarette paper skin” or skin atrophy with prominent underlying blood vessels.
Diagnosis is usually made on clinical findings; further diagnosis can be made with serological findings, clinical examination, and skin biopsy. To confirm the diagnosis, PCR or culture for detection of B. burgdorferi DNA can also be performed. The prognosis of the acute stage, if detected and treated early, is good. The prognosis of the chronic atrophic phase is poor as skin changes can’t be reversed completely.
How To Distinguish Acrodermatitis Chronica Atrophicans from Other Diseases
Distinguish Chronic Venous Insufficiency from ACA – Diagnosis
It is a condition in which veins have a problem returning blood to the heart. In this disease, there is a history of untreated varicose veins. The features that differentiate Chronic Venous Insufficiency from ACA are:
- Chronic Venous Insufficiency is caused by damage to the veins of the legs, while ACA is caused by bacterial infection with B. afzelii.
- Chronic Venous Insufficiency usually presents as bilateral lower limb swelling, which is painful, while ACA presents as red or bluish lesions and swelling, which is initially unilateral.
- Chronic Venous Insufficiency symptoms increase on standing and decrease on taking rest and elevation of legs, while ACA is not affected by a change in position.
It is diagnosed by physical examination and is confirmed with Duplex Ultrasound, which shows venous valvular insufficiency. There is no specific treatment for this disease. Treatment can only improve symptoms and the quality of life.
Distinguish Localized Scleroderma from ACA – Diagnosis
It is a rare, benign, autoimmune, and self-limited connective tissue disease of the skin, its underlying tissue, and internal organs. It has a high morbidity rate. The features that differentiate localized scleroderma from ACA are:
- ACA is a tick-borne disease, and localized scleroderma is suspected to be a spirochetal infection.
- Localized scleroderma presents as patches of thick, hard skin that are oval-shaped or have a waxy appearance with a bruise-like border, while ACA has unilateral bluish-red discoloration with prominent blood vessels.
- Localized scleroderma is a chronic connective tissue disease, while ACA is a chronic and late manifestation of Lyme borreliosis.
It is diagnosed by its appearance and can be confirmed by biopsy. It is self-limiting, but the damage caused to the skin while the disease is active can be permanent.
Distinguish Systemic Sclerosis from ACA – Diagnosis
It is a rare, systemic, and chronic autoimmune connective tissue disease. The symptoms of systemic sclerosis are CREST; Calcinosis, Raynaud’s phenomenon, Esophageal dysfunction, Sclerodactyly, and Telangiectasias. The features that differentiate systemic sclerosis from ACA are:
- Systemic sclerosis is an autoimmune disease, while ACA is caused by bacterial infection.
- Systemic sclerosis causes thickening and tightness of finger skin, puffiness, salt and pepper appearance of the skin, while ACA has an atrophic cellophane-like skin appearance with prominent blood vessels.
Systemic sclerosis is diagnosed with a physical examination, blood tests, and confirmed by the presence of autoantibodies in the blood.
Distinguish Frostbite from ACA – Diagnosis
Frostbite or cold injury is damage to the skin, nerves, and blood vessels below the top layer of skin caused by extremely cold weather. The features that differentiate frostbite from ACA are;
- Frostbite is more common on exposed parts of the skin like face, neck, hands, and feet, while ACA usually involves distal extremities and trunk, sparing the face, palms, and soles.
- Frostbite causes cold skin, numbness, color changing that eventually turns into hard skin, while ACA shows slowly increasing reddish-blue discoloration and swelling of the skin.
- Frostbite, if not treated properly, can cause serious damage that can lead to amputation of the affected part, while ACA, if left untreated, develops atrophy.
Frostbite is diagnosed based on signs and symptoms, recent exposure to cold, while to check the severity of the disease, X-rays, MRI, or a bone scan can be done.
Distinguish Erysipelas from ACA – Diagnosis
It is an acute bacterial skin infection. It usually affects the upper layer (dermis) of the skin and can involve superficial cutaneous lymph nodes. The features that differentiate erysipelas from ACA are;
- Erysipelas can be identified clinically as shiny, large, raised, red, tender, and indurated patches with distinct margins, while ACA shows multiple soft, bluish-red discoloration and subcutaneous swelling.
- Erysipelas is usually an acute unilateral skin infection, ACA is initially unilateral and then progresses into bilateral infection.
- Erysipelas involves the lymphatic system, while ACA is unlikely to involve lymph nodes.
Erysipelas is diagnosed based on history and clinical examination. It can be treated by taking rest, using cold compresses, and leg elevation.
Distinguish Superficial Thrombophlebitis from ACA – Diagnosis
It is a common thrombotic condition caused by clotting of venous blood in superficial veins under the skin. It is often benign and self-limiting. The features that differentiate superficial thrombophlebitis from ACA are;
- This condition occurs due to any acute trauma to the veins, such as while using IV lines, while ACA is a chronic and late manifestation of Lyme disease.
- Superficial thrombophlebitis causes pain, tenderness, swelling, and redness, while ACA presents as discoloration, hyperpigmentation, thin cigarette pipe-like skin.
- If left untreated, it can progress to pulmonary embolism or deep venous thrombosis, while ACA leads to flaccid atrophy of the skin.
It is diagnosed based on physical examination, blood tests, and ultrasound. Anticoagulants to prevent DVT must be used.
Distinguish Erysipeloid from ACA – Diagnosis
It is a very rare, self-limiting, and acute bacterial infection of damaged skin caused by Erysipelothrix rhusiopathiae. It can be localized or generalized. The features that differentiate erysipeloid from ACA are;
- It can involve any body part, but it mostly involves finger webs, while ACA usually presents on lower extremities.
- It is usually found in people working with fish and meat, while ACA is found in people having a history of infection with Lyme disease.
It is diagnosed with a history, clinical examination, biopsy, and PCR. It can be prevented by wearing gloves while handling fish or meat.
HOW TO PROTECT FROM ACA
As ACA is caused by infection with Lyme disease so
- People should take care going to tick-infested areas.
- They should wear full sleeves, long boots, long pants, gloves, and light-colored clothes.
- They should wear insect repellents, avoid contact with soil, and leaf litter.
- If there is any sign of redness, discoloration, or swelling after going to a tick-infested area, they should immediately consult a doctor.
