Contents
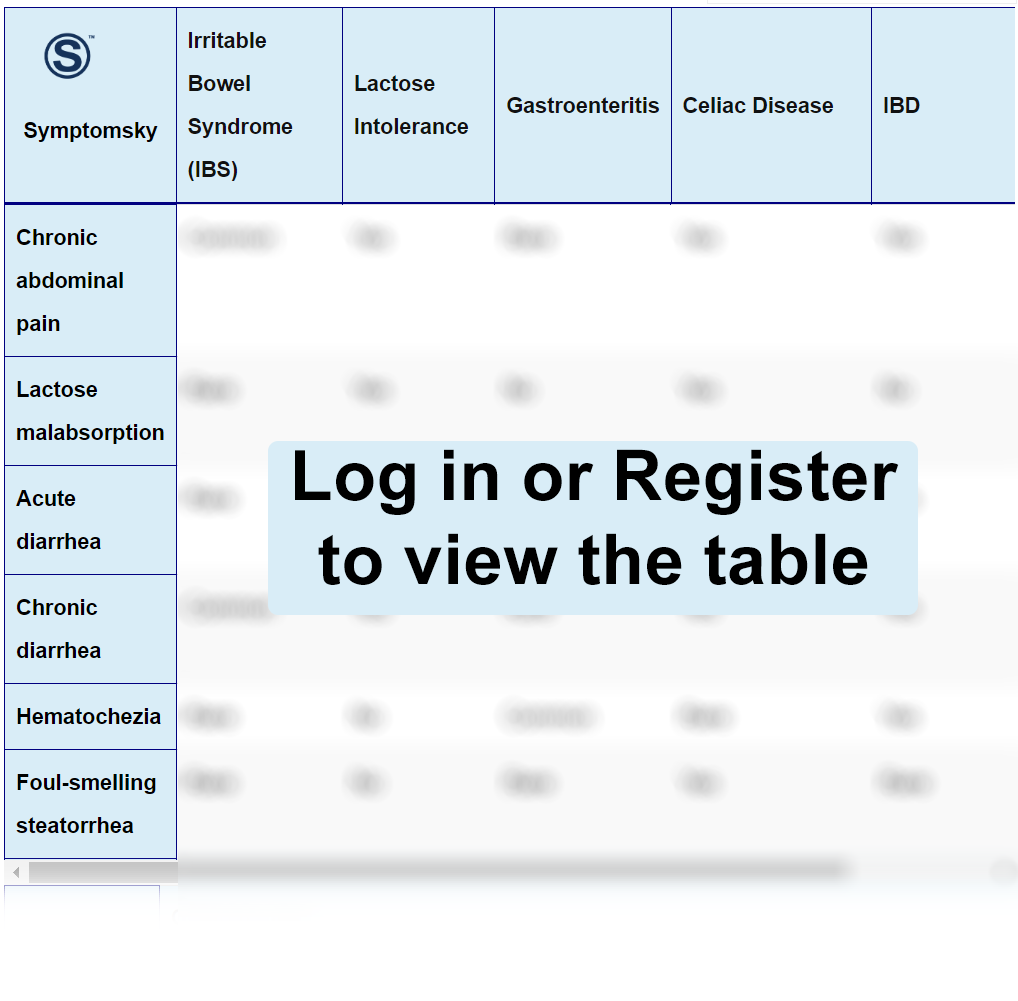
- 1 Abdominal Pain Differential Diagnosis Table:
- 2 How To Discern if Abdominal Pain Is The Cause Of The Following Diseases
- 2.1 How to Recognize that Irritable Bowel Syndrome (IBS) is Causing Abdominal Pain
- 2.2 How to Recognize that Lactose Intolerance is Causing Abdominal Pain
- 2.3 How to Recognize that Gastroenteritis is Causing Abdominal Pain
- 2.4 How to Recognize that Celiac Disease is causing Abdominal Pain
- 2.5 How to Recognize that Irritable Bowel Disease (IBD) is causing Abdominal Pain
- 2.6 How to recognize that Giardiasis is causing Abdominal Pain
- 3 Common Red Flags with Abdominal Pain
Abdominal Pain Differential Diagnosis Table:
Pain is defined as an unpleasant sensory experience. Establishing its origin has become a challenge with a great degree of difficulty since the abdomen presents diverse anatomical characteristics of the organs contained in this cavity. The causes of abdominal pain are multiple, and they are grouped according to pain and location, so it is important to understand the pathophysiology of pain.
Abdominal pain can be stimulated by three neural pathways:
Visceral pain: It is transmitted by c-fibers, which are found within the muscles, peritoneum, mesentery, and viscera. When a viscera is distended, this causes the local nerves to initiate an impulse which finally reaches the central nervous system. Since the nerve fibers of the different abdominal organs overlap and at the same time transmit sensory stimuli to both sides of the spinal cord, this pain is perceived by the patient as diffuse pain, or poorly characterized.
Somatic pain: It is transmitted by somatic nerves from the alpha fibers located within the parietal peritoneum in the muscle or skin unilaterally to the spinal cord. Because it is unilaterally located, it is well-localized and intense pain.
Referred pain: This type of pain involves afferent nerves from different sites but shares the same central pathway. These nerves are located at the level of the parietal pleura and the abdominal wall, meaning it is pain in an area far from the diseased organ.
A clinical history should be obtained as complete as possible since, in most cases of abdominal pain, the basis for an accurate diagnosis is the clinical history. It should include a complete description of the patient’s pain and the associated symptoms. Surgical and social history is of utmost importance as it can provide extremely important information during the diagnostic process.
The following questions should be asked about the pain:
Onset: It is important to know the characteristics of the onset of pain. Ask if the pain started suddenly. This may raise suspicion of a potentially serious pathology. Also, if the pain woke up the patient in the middle of the night, it should be considered serious. In these cases, we suspect serious potential intra-abdominal pathologies. The most important event in a vascular emergency is a ruptured abdominal aortic aneurysm. Other considerations may be a perforated ulcer, volvulus, or mesenteric ischemia.
Localization: This can be quite useful when orienting the etiology of the pain. It is one of the most important elements during this questionnaire since there are certain clinical pictures with semiological characteristics that must be known. For example, migratory pain from the epigastrium towards the right iliac fossa is likely to be acute appendicitis until proven otherwise.
Irradiation: This is nothing more than the transmission or spread of pain. There are typical semiological irradiations such as pancreatitis, starting as supraumbilical girdle-like abdominal pain and radiating dorsally.
Character: It is a somewhat difficult task to get the patient to decide the sensation of pain, but you should try to ask open questions without directly influencing the patient’s response. Ask them to describe the pain. There are associations that can guide us toward a diagnosis depending on the nature of the pain. Colicky pain is associated with intestinal obstruction or biliary pathologies, while dull pain is more associated with neoplastic pathologies.
Intensity: Ask the patient from 1 to 10 how much it hurts. High-intensity pain increases the suspicion of a serious cause; however, low to medium intensity pain does not totally exclude a serious disease, but the risk is lower.
Attenuating or aggravating factors: Conditions that increase or decrease pain are very useful in differential diagnosis. For example, pain that is triggered after ingestion of high-fat meals and is located in the upper abdomen suggests a biliary pathology.
Accompanying symptoms: Ask the patient if the abdominal pain is accompanied by any other symptoms such as fever, vomiting, diarrhea, hematemesis, melena, or hematochezia.
How To Discern if Abdominal Pain Is The Cause Of The Following Diseases
How to Recognize that Irritable Bowel Syndrome (IBS) is Causing Abdominal Pain
Irritable Bowel Syndrome is a functional gastrointestinal disorder. Abdominal pain in Irritable Bowel Syndrome is characterized as a diffuse pain that is mostly located in the lower abdomen and does not radiate. It is oppressive, cramping type, sometimes can be stabbing, and the pain ranges from mild to moderate in intensity. Something very characteristic is that it is relieved after defecation and is also accompanied by tympanism or meteorism.
Another very common characteristic of this syndrome is that the abdominal pain is chronic. However, this does not mean that the disease progresses to more severe conditions. The patient will also present changes in their evacuatory pattern (diarrhea or constipation) as well as the presence of mucus in the stool.
How to Recognize that Lactose Intolerance is Causing Abdominal Pain
Lactose Intolerance is a condition caused by malabsorption of lactose due to a lactase deficiency. Abdominal pain in Lactose Intolerance begins within half an hour to two hours after ingesting food or beverages containing lactose, is located in the lower half of the abdomen and periumbilical area, is accompanied by bloating, diarrhea, flatulence, and nausea.
How to Recognize that Gastroenteritis is Causing Abdominal Pain
Abdominal pain caused by Gastroenteritis is a colicky pain with diarrhea in large quantities and in some cases may cause hematochezia. It presents dehydration, vomiting, nausea, and fever.
How to Recognize that Celiac Disease is causing Abdominal Pain
Abdominal pain caused by Celiac Disease is a poorly defined pain that manifests itself after eating foods containing gluten, is accompanied by abdominal distension, flatulence, and alternating changes in the patient’s bowel movements, i.e., the patient may be totally constipated as well as have diarrhea. The stools are foul-smelling, pale, and greasy. It may be accompanied by other symptoms such as fatigue due to iron deficiency.
How to Recognize that Irritable Bowel Disease (IBD) is causing Abdominal Pain
Irritable Bowel Disease causes chronic lower abdominal pain, increased frequency of bowel movements, diarrhea, bloody or black stools, weight loss, anorexia, joint inflammation, and symptoms worsened over time.
How to recognize that Giardiasis is causing Abdominal Pain
Giardiasis abdominal pain is abrupt onset cramping accompanied by nausea, vomiting, and watery diarrhea predominantly in the morning or postprandial. Five to ten liquid, fatty, fetid, and explosive diarrhea, may be permanent or intermittent and lasts three to four days.
Common Red Flags with Abdominal Pain
Unlike the usual physical examination steps, auscultation should precede palpation when performing an abdominal physical examination, since palpation before auscultation can cause irritation and significant pain in healthy patients.
Alterations in vital signs are very frequent and are mostly related to the severity of the condition; however, the presence of normal vital signs does not exclude a serious diagnosis.
Fever is used as a parameter of infectious cause or secondary complication. Fever may be absent, especially at the beginning of an infectious condition. That is why it is necessary to be aware that an infectious cause or a complication cannot be ruled out in an afebrile patient because it may be that it just has not started.
The choice of laboratory tests will vary according to the clinical situation: a complete blood count is appropriate if an infection or blood loss is suspected. In patients with right upper quadrant pain, liver biochemistry tests are important. In patients with epigastric pain, it is recommended to request C-reactive protein as it is very useful for diagnosis in case of suspected acute appendicitis. A urinalysis should be requested in patients who present with hematuria, dysuria, and flank pain as accompanying symptoms.
A pregnancy or urine test should always be considered in women of childbearing age who present to the emergency department for abdominal pain.
